Background: In 2021 there were over 80,000 opioid overdose deaths. Studies show that inpatient hospitalizations are a vital moment in treating patients with opioid use disorder (OUD). Initiation of opioid agonist therapy (OAT: buprenorphine or methadone) is associated with a profound mortality benefit, with some studies suggesting a number needed to treat of less than 5. A barrier to buprenorphine treatment in the hospital setting is that patients must be in mild-moderate withdrawal prior to starting buprenorphine (induction). This is done to avoid precipitated opioid withdrawal (POW) wherein buprenorphine, a high-affinity, partial agonist of the µ-opioid receptor (MOR) abruptly displaces full agonists causing unpleasant symptoms.“Microinduction” is a novel process that entails administering very low doses of buprenorphine at fixed intervals such that the displacement of full agonist opioids is so gradual that POW symptoms are clinically attenuated. This removes the need for a withdrawal period prior to a buprenorphine induction as patients are able to continue taking full agonist opioids as buprenorphine reaches therapeutic levels. This is a new practice and has shown great potential in facilitating inpatient inductions.
Methods: We reviewed charts of 60 patients who received IV buprenorphine over a 10-month period at a tertiary academic medical center. Inclusion criteria was use of IV buprenorphine for microinduction; exclusion criteria was any other use of IV buprenorphine. A manual chart review obtained clinical opiate withdrawal scale (COWS) and pain scores over a 6-day period starting the day prior to microinduction. COWS measures opioid withdrawal severity on a scale from 0-48; pain scores were self-reported on a scale of 0-10. Two researchers performed a review and compared data to ensure accuracy. 49 patients met inclusion criteria. Two treatment groups were identified: a “slow regimen” (11 patients) received buprenorphine 2x daily on day 1, and a “standard regimen” (38 patients) received buprenorphine 4x on day 1. Daily COWS and pain scores were aggregated within both groups using mean values.
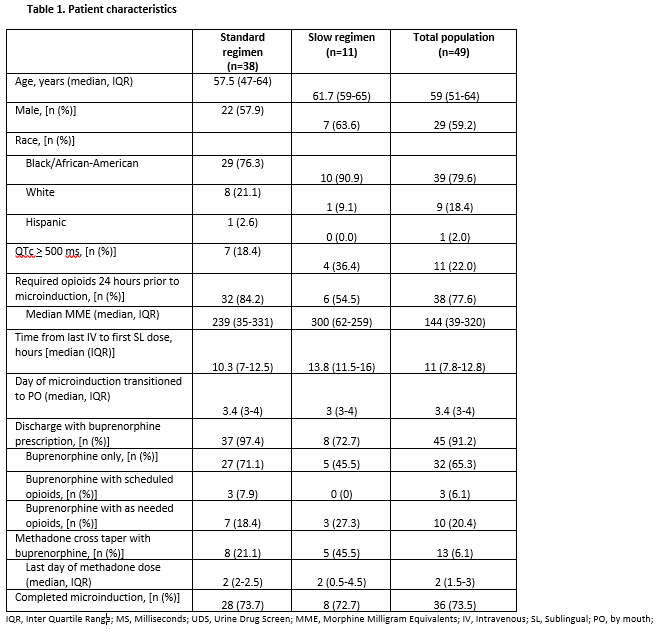
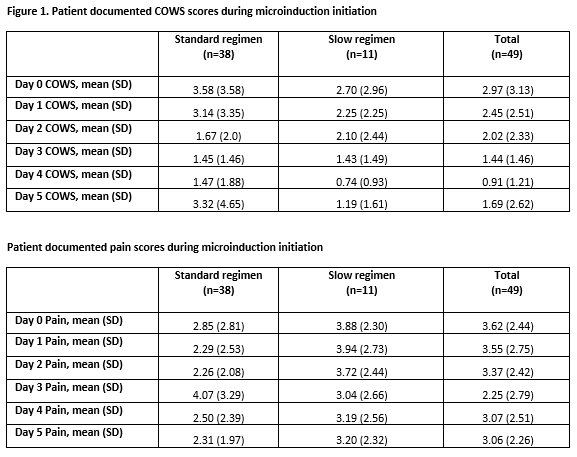
Results: Patient characteristics in Table 1 include age, sex, race, patients discharged with buprenorphine, and patients who successfully completed the microinduction. Over 70% of patients in both groups successfully completed the microinduction.Figure 1 depicts the aggregated daily COWS and pain scores in both groups. Day 0 denotes the time from midnight the day prior until buprenorphine administration on day 1 to contrast pre and post buprenorphine scores. Subsequent days are in midnight-to-midnight intervals. Day 0 average COWS was 2.97; Day 5 was 1.69. Day 0 average pain score was 3.62; Day 5 average was 3.06. COWS and pain scores remained low for all patients throughout the process.
Conclusions: The use of IV buprenorphine for inpatient microinductions was well tolerated with regards to withdrawal symptoms and pain. Over 70% of all patients successfully completed microinduction, with only 1 self-directed discharge. As the opioid epidemic worsens, hospitalizations are crucial in initiating OAT, particularly buprenorphine, which has galvanized hospitalist-led efforts to manage OUD. Microinduction enables patients to start buprenorphine while still on full agonist opioids or having recently taken heroin or non-pharmaceutical fentanyl. We believe IV buprenorphine will be key to the management of OUD in hospitals both for microinductions and potentially as part of standard induction practices.