Background: The VA, like many health care systems, seeks to meet the needs of a rapidly growing older adult population. The transition from hospital to post-hospital care – particularly in older adults- is increasingly common, but unfortunately is high-risk and low-value. Further, 85% of older adults choosing a skilled nursing facility had a higher-quality facility nearby, and 50% had 5 or more of higher quality. Thus, more can be done to improve decision-making about post-acute care (PAC) by patients, caregivers, and clinicians. In particular, improved tools that facilitate the choice of high-value skilled nursing facility (SNF) or home health (HH) agencies could improve outcomes of Veterans and lower costs. We sought to identify opportunities to improve decision making about PAC from the perspective of key operational VA stakeholders.
Methods: We conducted eighteen semi-structured interviews to understand the perspectives of VA operational stakeholders regarding the current PAC decisional context; available PAC decision tools; gaps and barriers in the transitions of care; and potential design considerations for system-level PAC decision tools. We used a purposive snowball sampling approach to identify relevant leaders at the national level from the following offices: Office of Community Care, Geriatrics and Extended Care, Rural Health, Nursing Services, Social Work, Health Equity, and Quality and Safety. Interviews lasted approximately one hour and were transcribed and then coded by two researchers using a group-based consensus approach to inductively identify themes.
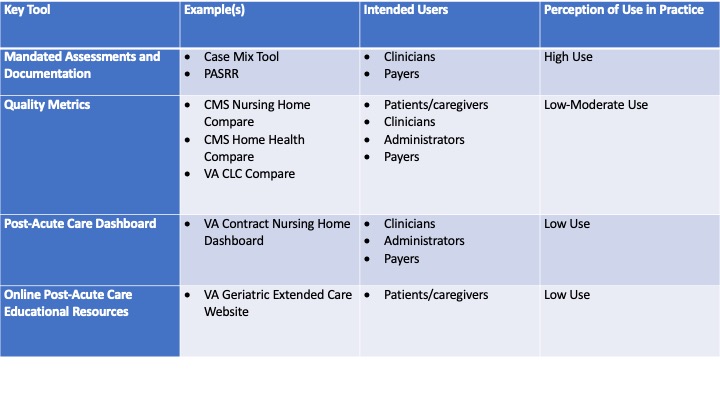
Results: Our sample consisted of 56% female interviewees; their median time spent in their current role was 4 years and the median time spent at the VA was 20 years. They placed a signficiant emphasis on need to improve transparency on the utilization, quality, and cost of PAC services used by Veterans to inform policy, budget, and resource allocation. Overall, key stakeholders reported few available tools to improve PAC decision making at a micro- or a macro-level. Examples of macro-level tools included: mandated assessments/documentation, quality metrics, and online PAC educational resources (Table 1). They emphasized five operational gaps at a VA system macro-level, including: (1) measuring quality of VA and non-VA skilled nursing facilities, home health agencies, and other PAC providers; (2) ensuring veterans are aware of all PAC options; (3) maximizing inter-departmental coordination; (4) identifying which PAC providers to include within the VA network; and (5) monitoring hospital-PAC use patterns at a national and regional level -especially from a cost and a health equity standpoint. To overcome these gaps, stakeholders suggested several design considerations for future tools.
Conclusions: To improve PAC decision-making and increase PAC value, VA operational leaders emphasized system-level approaches that increase transparency and potentially allow the system to influence – or narrow- the PAC network and PAC choice. However, few existing tools were identified that could serve this purpose. Many health care systems seek to improve post-acute care value for recently-discharged patients given their outcomes are increasingly financially tied to hospital payments. Developing system-level tools that are effective for improving PAC value across the population of patients in a health system – without unintended consequences related to autonomy – may be a promising avenue to improve outcomes.