Background: In current times, physicians are working to older ages, lending experience and knowledge that benefits both patient care and education. Recent findings demonstrate advanced age as a risk factor for severe morbidity and mortality from serious acute respiratory syndrome-coronavirus-2 (COVID-19), placing older physicians at high-risk during the current pandemic. Pediatric hospitalists frequently care for children with various respiratory illnesses, therefore older providers are likely to be exposed to patients with known or unknown COVID-19 infection. The objective is to define the current state of practice regarding modifications to work hour requirements and patient encounters for late career (over 50 years of age) pediatric hospitalists in light of the COVID-19 pandemic.
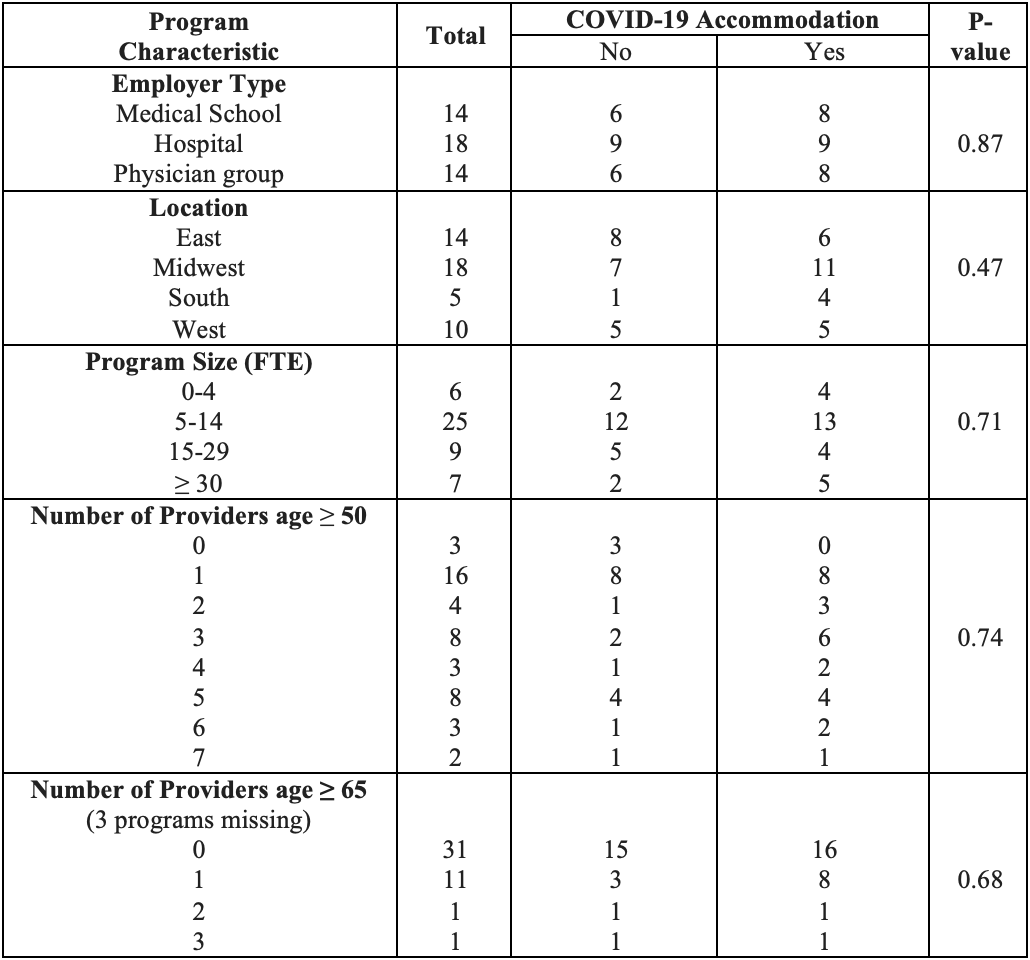
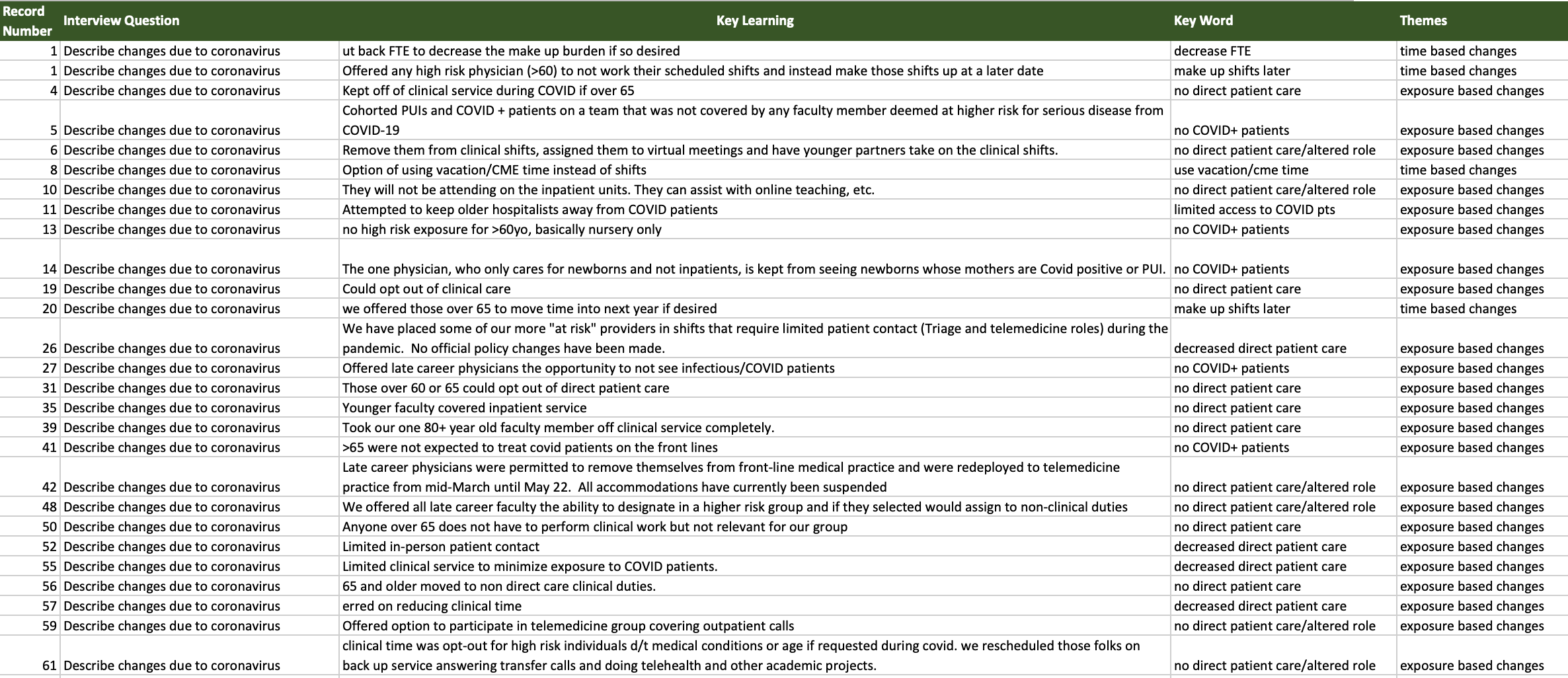
Methods: This descriptive mixed method study used an anonymous electronic cross-sectional survey sent to the American Academy of Pediatrics Hospital Medicine Division Chiefs listserv between May and June of 2020. The survey used Yes/NO, multiple-choice and open-ended questions to assess schedule accommodations made due to COVID-19 for late career pediatric hospitalists. Grounded theory was used to analyze responses to open-ended questions, with questions coded, developed into themes by 2 investigators, and compared until consensus was achieved (Image 1). The Fisher exact test examined the association of program characteristics with COVID-19 accommodations.
Results: Surveys were completed by the directors of 47 programs, including 43 (91%) with members ages 50 to 64 years, and 13 (28%) with members ≥ 65 years. The corresponding total of 982 individual hospitalists included 117 (12%) ages 50-64 years and 15 (1.5%) ages ≥ 65. Employer types included hospital, medical group, or medical school (Table 1). Of the programs with hospitalists 50-64 years of age, 60% made accommodations; and the number increased to 77% for programs with providers age 65 and over. No statistical difference was noted in accommodations when compared by location, employer type, program size, or total number of physicians employed over the age of 50 or 65 (Table 1). Qualitative analysis revealed 2 major themes: time-based (15%) and exposure-based accommodations (85%). Time-based accommodations included examples such as “we offered those over 65 to move (clinical shifts) into next year”. Examples of exposure-based modifications included “limited in-person patient contact” and “kept off of clinical service during COVID if over 65”.
Conclusions: While nearly all surveyed programs that responded to the survey employed hospitalists over the age of 50 years, only one-fourth had a member over the age of 65. COVID-19 accommodations increased from 60% to 77% when employees over the age of 65 were present. Changes made were either time-based or exposure-based, with exposure-based changes having a higher prevalence. In order to retain the valuable input from late career hospitalists, programs will need to carefully consider how to best utilize these practitioners safely over the remaining course of the pandemic.