Background: The practice of routinely ordering daily labs not based on clinical indication on patients in the hospital is a wasteful clinical practice. Routine daily labs can also lead to patient harm by causing pain and iatrogenic anemia, and can burden laboratory staff resulting in increased lab reporting times. Raising awareness about unnecessary lab orders is a major interest of hospitals nationwide, with an increasing focus on high-value care. Decreasing unnecessary lab ordering results in decreased costs and allows for reallocation of hospital resources, which can be of particular importance to hospitalists providing care for underserved populations within a safety-net hospital. We present a project aimed at reducing unnecessary lab testing within a large inpatient medicine ward service.
Methods: Our study was conducted at a 600-bed publicly-funded safety net hospital. Our targeted labs were CBC with and without differential, CMP, BMP, Magnesium and Phosphorus levels. Our interventions targeted residents rotating on the general medicine service, the night-float residents, and the attending physicians on service. A standardized presentation encouraging purposeful lab use and discussing the pitfalls of daily lab orders was given to the residents every three weeks. The same information was disseminated to night-float residents via weekly texts, email reminders, and posters placed in all on-call rooms. The project’s goals were presented at inpatient hospitalist meetings to rounding attending physicians. Finally, we adjusted the electronic medical record system (EMR) by adding the option of “CBC without differential” to the admission order set that is available to the residents, when previously it was not an option. We collected data prospectively and presented results monthly.
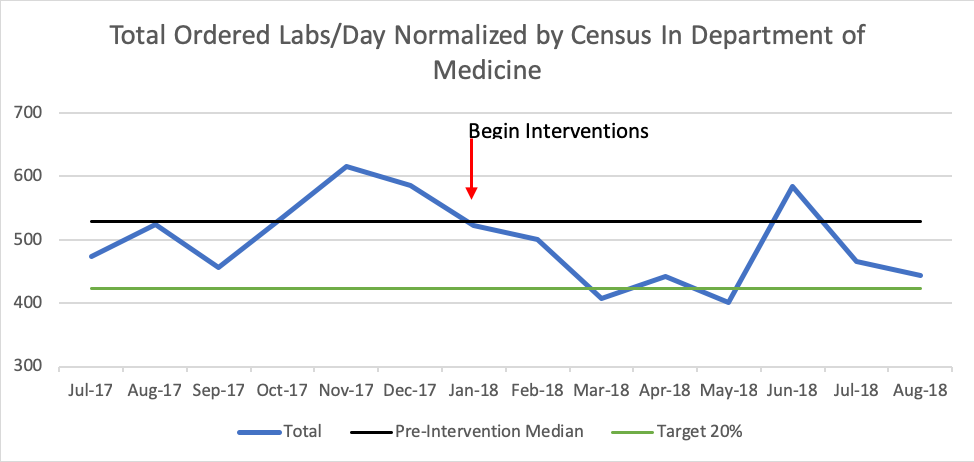
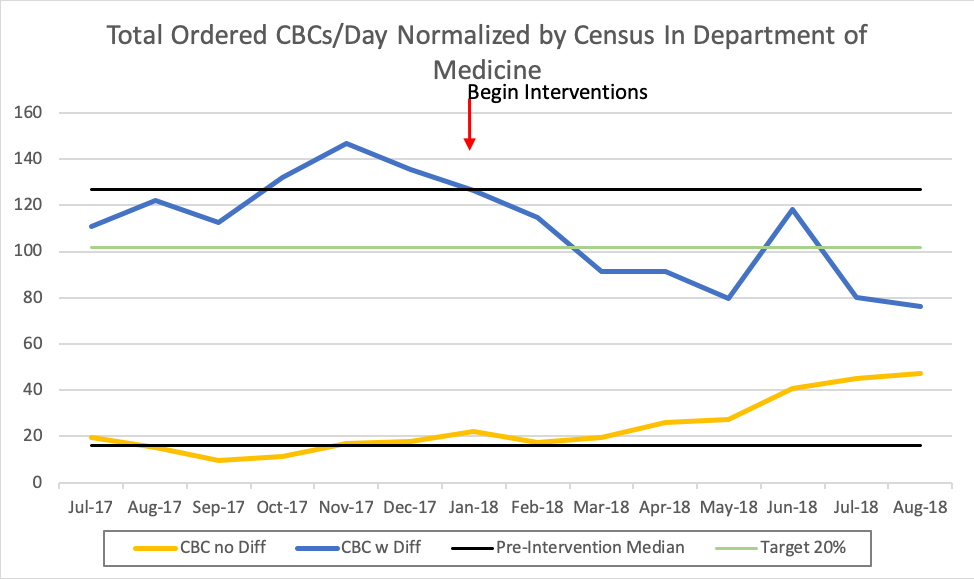
Results: The pre-intervention baseline median of labs ordered by inpatient internal medicine residents over six months was 529 labs/day, which given an average census of 256 patients is 2.06 labs/patient-day. After eight months of our intervention, we achieved an average 14.2% reduction in labs per day (454 labs/day or 1.77 labs/patient-day). The “CBC with differential” and “CBC without differential” pre-intervention normalized medians were 127 labs/day and 16 labs/day, respectively. Post-intervention, the “CBC with differential” and “CBC without differential” medians were 91 and 27, respectively. This represents a 28% reduction in “CBC with differential,” with a concurrent 69% increase in “CBC without differential.” Overall, there was a 17.5% decrease in total number of CBCs with or without differential ordered.
Conclusions: Multiple interventions including resident education, promoting attending awareness, and adjustments to the EMR resulted in decreased total labs ordered over the study period. In particular, we saw a decrease in “CBC with differential” with a concurrent increase “CBC without differential,” with an overall decrease in the total number of CBCs ordered. This particular change in ordering habit is likely largely due to the EMR adjustment made, given the significant degree of change when compared to the other labs of interest. This demonstrates the importance of prioritizing targeting structural changes, which is of particular importance to hospitalists, who have the opportunity to identify wasteful and harmful practices in the inpatient setting that could benefit from intervention. Future studies should investigate more targeted interventions aimed at decreasing wasteful practice habits.