Background:
Patients are often discharged from hospitals before test results are finalized. Physician awareness of test results finalized after hospital discharge is poor and is an important patient safety concern. We aimed to determine the impact of a computerized test result management application (Hospital Results Manager, HRM) on physician awareness of potentially actionable postdischarge test results.
Methods:
The outpatient computerized test result management application for 2 academic medical centers (Results Manager, RM) was modified to allow inpatient physicians to (1) track tests pending at discharge, (2) review finalized results once available, and (3) provide inpatient physicians the option of electronically forwarding these results to the patient's primary care physician (PCP). Inpatient results were otherwise unavailable to the PCP in RM. We randomized inpatient physicians at both hospitals to HRM or usual care to determine the effect of HRM on inpatient and PCP awareness of potentially actionable postdischarge test results. We measured satisfaction and frequency of use of this application as secondary end points.
Results:
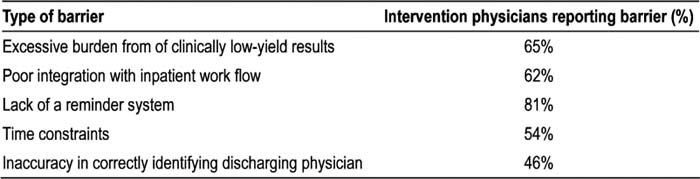
The study found that 46.9% of intervention physicians (95% Cl 33.0%–60.9%) and 34.2% of control physicians (95% Cl 19.6%–48.7%) were aware of potentially actionable postdischarge test results. Only 1 physician in the intervention group reported using HRM to become aware of the finalized postdischarge test result. HRM was never used by 48% of inpatient physicians randomized to the intervention. Eighty‐five percent of intervention physicians reported barriers prohibiting the use of HRM (Table 1). Physicians unanimously agreed that an ideally designed computerized results management application would be valuable for managing pending test results at the time of discharge.
Table 1. Types of Barriers Prohibiting Intervention Physician from Using HRM to Manage Postdischarge Test Results
Conclusions:
A computerized results management application did not improve physician awareness of postdischarge test results because it was not used. Key lessons to consider in designing future applications include: (1) a mechanism of filtering clinically low‐yield post‐discharge test results, (2) integration with inpatient work flow, (3) an alert system to remind physicians of finalized postdischarge results, (4) clear delineation of the responsibility for managing postdischarge test results, and (5) accurate identification of the discharging physician.
Author Disclosure:
A. Dalai, none; E. Poon, none; A. Karson, none; T. Gandhi, none; C. Roy, none.