Background: Advance care planning (ACP) helps patients plan end of life care in accordance with their goals and values, but is often performed too late and infrequently. Hospitalists play an important role in delivering ACP for patients admitted for serious illnesses, but often cite competing inpatient priorities, lack of time and training, and uncertainty about prognosis as barriers. An analysis at our institution revealed that non physician providers, such as nursing, social work, and rehabilitation services, demonstrate strong desire to contribute to ACP, but do not feel empowered to do so. We describe the design and implementation of a multidisciplinary, team-based approach to ACP that leverages artificial intelligence AI. We previously developed a machine learning (ML) model that identifies patients at high risk for dying within 3-12 months of their hospitalization. These predictions enable consistent identification of patients who may benefit from ACP. We incorporate these predictions into a human-in-the-loop workflow that includes hospitalists, nursing, social work, and rehabilitation services to deliver ACP.
Purpose: Use AI to enable a multidisciplinary team based approach to effectively deliver advance care planning.
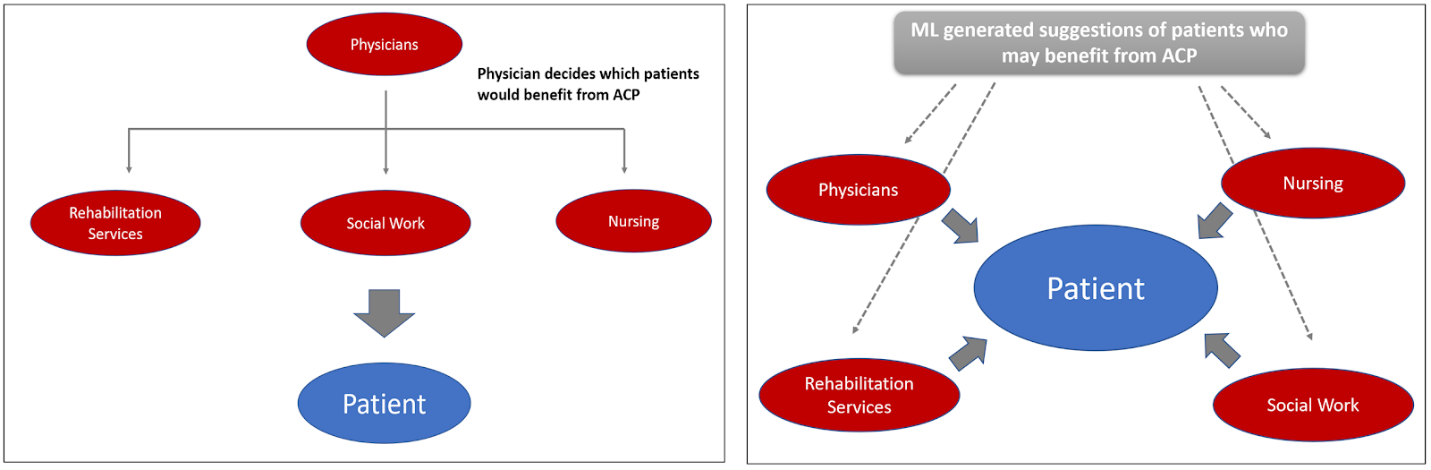
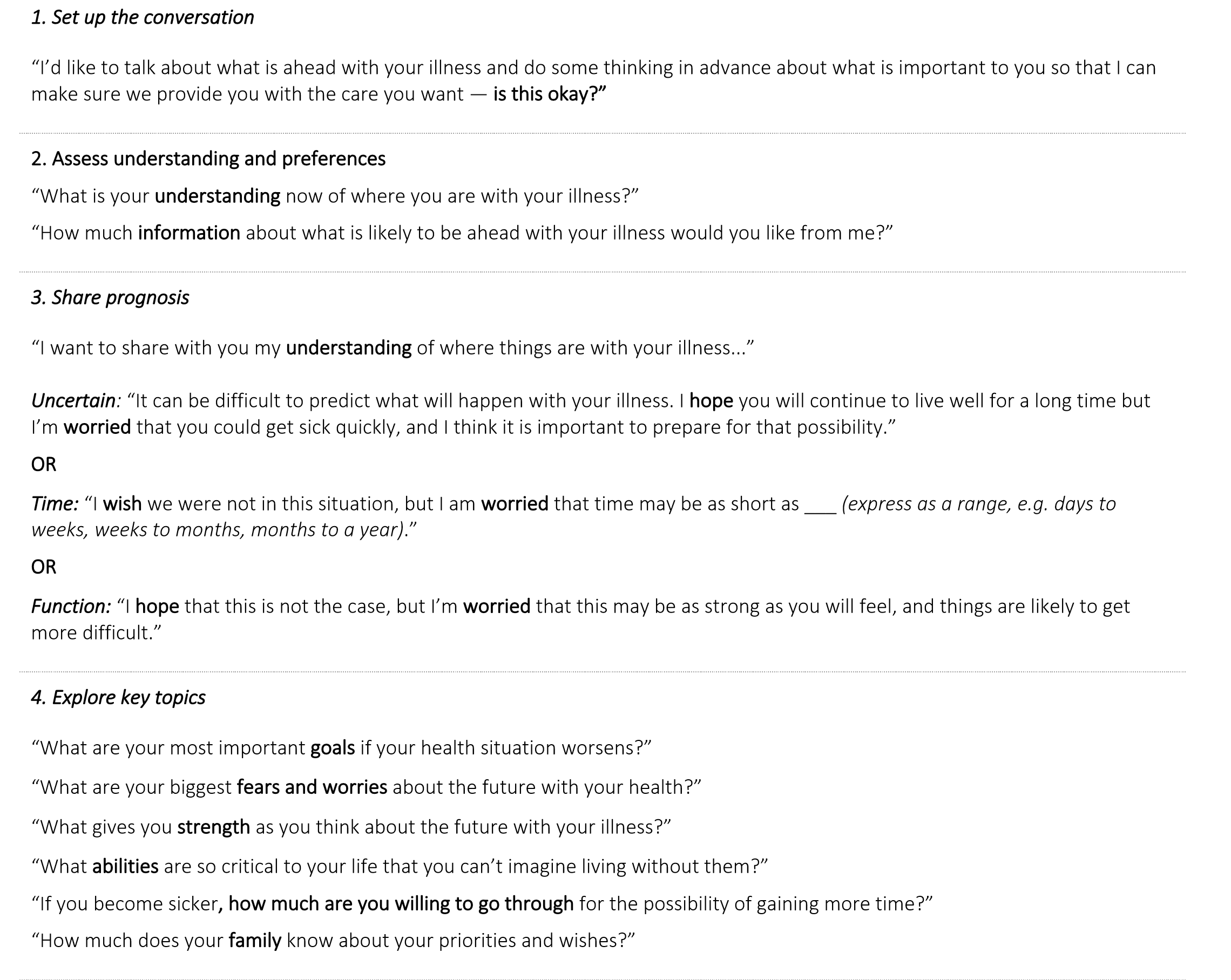
Description: This workflow was implemented in Fall 2020 on the general medicine resident teaching wards in partnership with select nursing units at a tertiary care center. Several key drivers were identified: a shared understanding across the team of how to identify which patients need ACP, a shared workflow for conducting and documenting ACP, and empowerment of each team member rather than only the physician to initiate the ACP process. We completed participatory design sessions and employed a plan-do-check-act (PDCA) process to iteratively design and implement a new AI enabled workflow for ACP (Figure 1). A ML model generates a list of candidate patients for ACP whose predicted probability of 3-12 month mortality exceeds 25%. For transparency, this list is visible to all providers and triggers a multidisciplinary team driven workflow, where nursing, social work, and rehabilitation services along with physicians can initiate portions of ACP and update a shared ACP documentation module in the electronic health record. All providers were trained to conduct ACP using a standardized communication tool, the Serious Illness Conversation Guide (SICG) (Figure 2), designed by Ariadne Labs. While prognosis discussion is reserved for the physicians, non physician team members can initiate other sections of the SICG–such as the patient’s understanding of illness and their hopes, worries, and fears–and request that the physician discuss prognosis with these selected patients. We observed significant increases in participation from nursing, social work, and rehabilitation services providers who have previously not initiated ACP conversations. We did not receive any concerns that the list of candidate patients for ACP was generated by AI. There was broad agreement regarding the appropriateness of the lists among users, but key barriers to implementation remain, including confusion around how to access the ACP documentation module and how to delegate ACP across multiple providers.
Conclusions: We describe the design and implementation of an effective AI-enabled workflow to enable a team-based approach to advance care planning (ACP) for hospitalized patients that includes physicians, nursing, social work, and rehabilitation services.