Background: Early discharges from inpatient units improve throughput from the Emergency Department (ED) and reduce ED boarding. ED boarding increases patient safety events, provider burnout, and decreases patient satisfaction. Multidisciplinary communication between hospitalists, nursing staff and case management is essential for facilitating early discharges from inpatient medicine units. Such communication frequently requires in-person care coordination rounds (CCRs) on medicine floors. The disruption to in-person meetings due to COVID19 and the emergence of secure chat-based communication via electronic medical records such as Epic TM provides an opportunity for virtual CCRs. We present our experience with virtual CCRs and their impact on discharges by noon.
Methods: Our facility is a 700-bed safety net hospital and level 1 trauma center that operates at or above capacity. We deploy 13 hospital medicine teams that see an average of 185 patients on 6 medicine floors. Prior to April 2022, each team was assigned to 1-2 floors. Patients were admitted to a team, and the bed planner prioritized patients to the floor assigned to that team. Only 30-40% of patients were correctly localized in this model. In April 2022, we worked with bed planners to localize patients on one medicine unit cared for by 2 direct care hospital medicine teams. We also initiated Epic TM secure chat-based, discharge focused multidisciplinary rounds on this floor. Epic TM secure chat is a messaging service that allows multiple healthcare workers (HCWs) to securely communicate about patients. Members of the care team can initiate a secure chat and add other HCWs to the same chat. Virtual CCRs were initiated on the pilot unit by the unit Patient Care Coordinator (PCC). The PCC, who is a registered nurse, initiated separate secure chats with the physicians and advanced care providers of each of the two hospital medicine teams. Case managers, social workers and charge nurses were added to the chat. Discharge readiness of each patient was discussed, along with discharge barriers. These virtual rounds took no longer than 10 minutes per team. The PCC escalated discharge needs to other disciplines such as physical therapy and respiratory therapy after virtual rounds as needed.
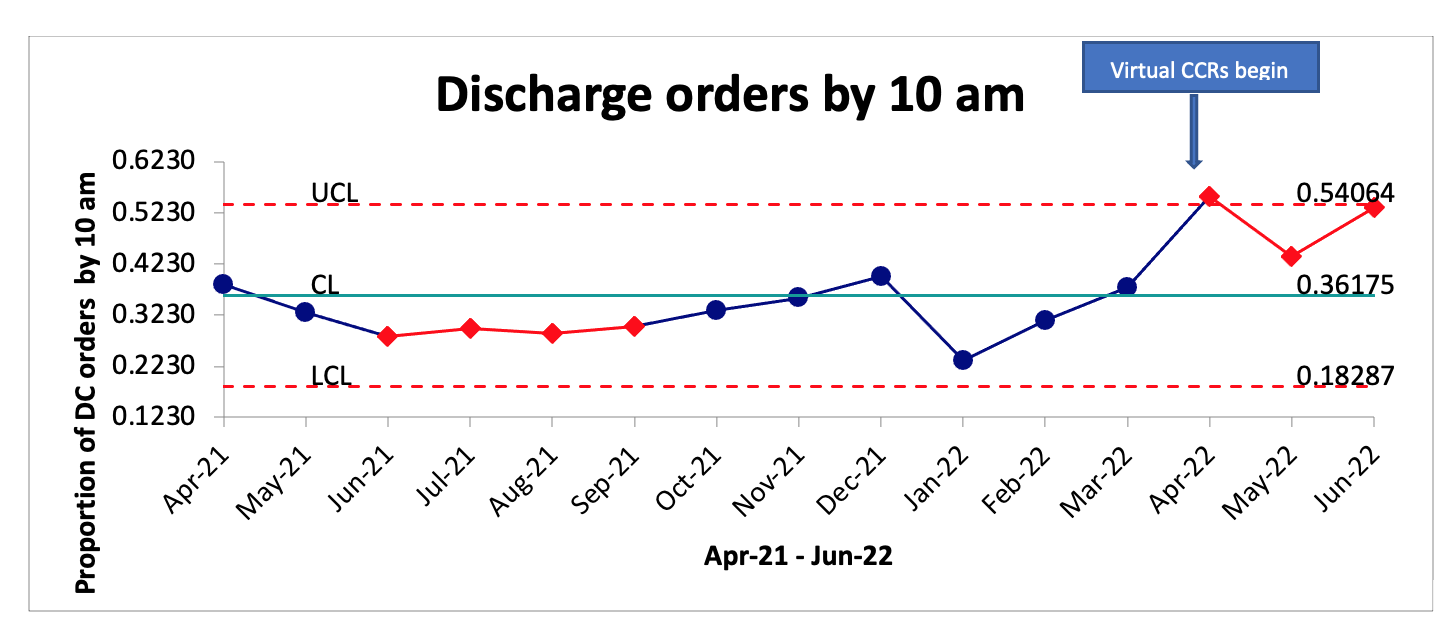
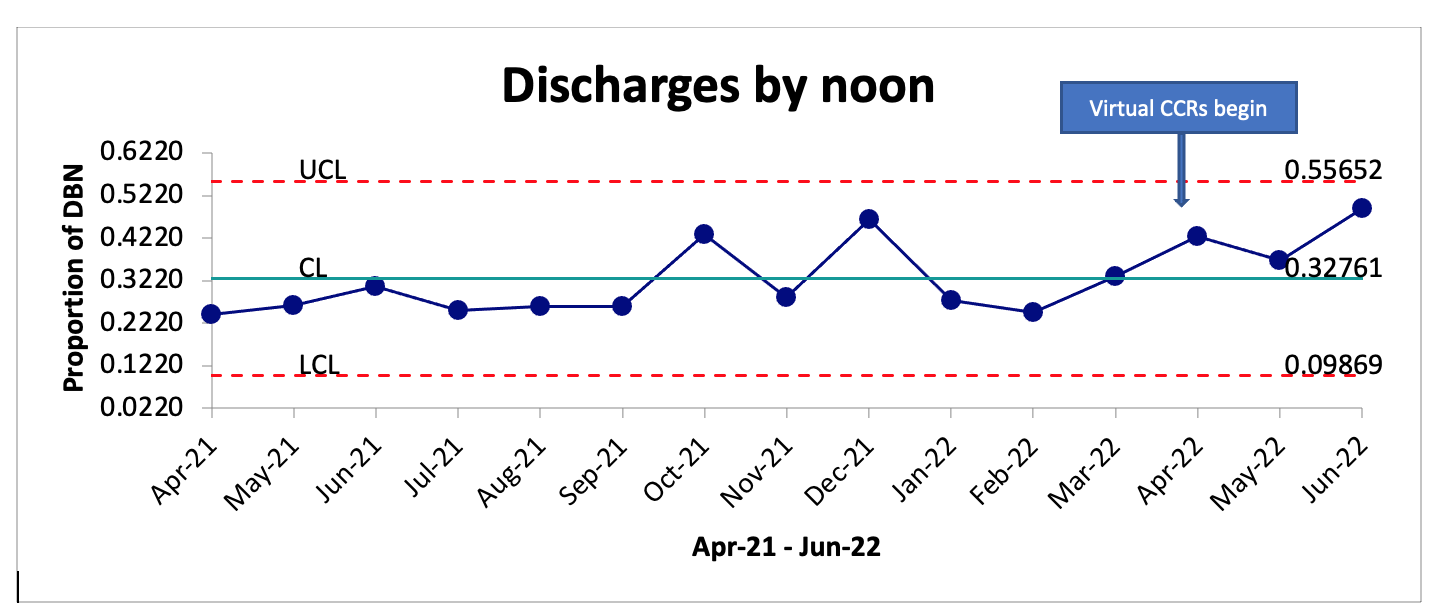
Results: We present the results of the first 3 months of this pilot. The average proportion of patients on the two teams localized to the pilot unit was 80%. The proportion of discharge orders placed by 10 am on the two teams localized to the pilot unit increased from 29% (300/1018) during April 2021-March 2022 to 50% (141/282) during April 2022-June 2022, p-value < 0.00001. The proportion of discharges by noon increased from 31.3% (272/871) to 44.3% (131/296), p-value 0.0005. Five of thirteen (38%) eligible hospitalists responded to a survey on their perception of virtual CCRs. All respondents “agreed” or “strongly agreed” that virtual CCRs should be continued. All respondents also either “agreed” or “strongly agreed” that secure chat-based CCRs helped escalate barriers to patient discharge and reduced the time taken to discharge a patient.
Conclusions: Virtual CCRs with hospitalists, case managers and nurses localized to a medicine unit increased the proportion of patients discharged by noon. The virtual CCRs were brief, structured, and discharge focused. In addition, PCCs were empowered to escalate and resolve multidisciplinary logistical barriers to discharge. Secure chat-based care coordination rounds are now the standard for all 8 direct care hospital medicine teams in the morning.