Background: Hospitalist providers are the backbone of inpatient medicine and are the ideal audience for hospital-driven metrics given their direct and constant care of hospitalized patients. However, these metrics often seem ambiguous, resulting in frustration and dismissal. Guiding hospitalist providers through less commonly understood topics such as utilization review determinations (nuances of observation/inpatient status), high yield clinical documentation, and denials creates increased engagement and enthusiasm towards these initiatives.
Purpose: The purpose of an innovation around teaching hospitalist providers the nuances of hospital-driven metrics is multifaceted. Hospitalist providers have personal goals that they are trying to reach, typically displayed on division dashboards and even possibly tied to financial incentives. At the same time, the hospital is constantly striving to improve quality-driven metrics such as decreasing observed over expected length of stay and mortality. Through providing the nuts and bolts of these seemingly ambiguous topics, hospitalist providers can improve their personal goals and, simultaneously, the hospital’s goals. Furthermore, a better grasp of these initiatives can help hospitalist providers speak the “language” that hospital leadership will understand.
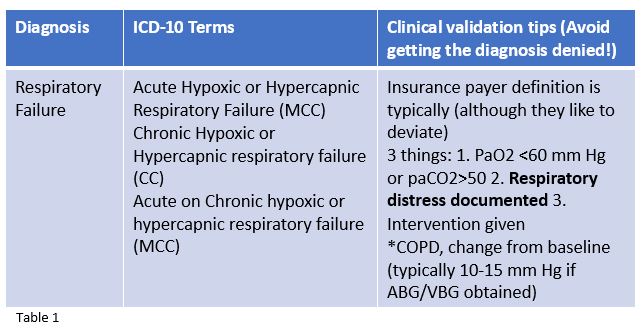
Description: A four-part hospital medicine virtual learning series was created to teach hospital medicine providers how to implement utilization review tactics through an understanding of admission determinations, maximize documentation to improve personal and organizational quality metrics, and improve success when fighting denials. The first session aimed to discuss observation and inpatient status through documentation strategies and impact on length of stay, a commonly misunderstood hospital metric. The second session tackled denials, both of inpatient status and of ICD-10 diagnoses, with targeted areas to implement for improved success. The last two sessions reviewed the strength of clinical documentation’s ability to impact expected mortality, length of stay, and cost. Specific examples of optimized documentation were given, such as in Respiratory Failure, as shown in Table 1. These sessions were delivered by two physician advisors, both of whom are also hospitalists and guide the hospital in these areas in their administrative roles. Surveys were given after each session to gain feedback and improve directives.
Conclusions: Survey data of the learning series revealed that 100% of participants either agreed or strongly agreed that the conference met their learning needs and gave them new information they expected to use on an ongoing basis. The majority of participants felt that the information provided would change their current practice (86% 18/21). Hospitalists providers have a vested interest in hospital driven metrics and are interested in understanding them when given the opportunity. Given the power of these metrics, becoming well versed in these strategic efforts keeps hospitalist providers in control of their benchmarks and the derivatives of it. Next steps in our initiative will be to make the virtual series as interactive as possible, including polling options and small group breakouts if able. Tracking individual metrics will make this initiative even more successful in the future.