Background: Mental fatigability is a measure of an individual’s susceptibility to increased mental fatigue resulting from engaging in physical and/or mental activities. Mental fatigability is important in hospitalized patients because it is has been shown to be associated with reduced physical activity levels, and reduced activity directly contributes to hospital associated disability and reduced functional recovery post hospitalization. Moreover, mental fatigability is important in hospitalized patients because it can influence the cognitive functions (e.g. attention, self-efficacy, emotional responsivity, reasoning, memory) that are needed to actively engage with hospital providers in making authentic and optimal decisions about care during hospitalization. Hospitalized patients with anemia may be at a particular risk for increased mental fatigability and its untoward consequences, since anemia itself is independently associated with both reduced physical fatigue and decreased cognitive function (as a result of decreased tissue oxygenation). However, there is no data describing whether there is an association between anemia (patient’s hemoglobin (Hb) level) during hospitalization and their mental fatigability level. Therefore, the purpose of this study was to collect data on and test for an association between patient’s Hb levels during hospitalization and mental fatigability.
Methods: From 7/2017-2/2019 hospitalized general medicine patients with a Hb < 10g/dL were approached for an inpatient interview at hospital admission. Patients with a diagnosis of dementia were recruited for the study but excluded from analysis. Mental fatigability was measured using the Pittsburgh Fatigability Scale (PFS), a validated instrument for measuring mental fatigue in the context of specific activities of fixed duration. PFS scores range from 0-50, with higher scores indicating greater mental fatigability (worse cognition for any given activity). Patients’ Hb values and clinical data were abstracted from hospital administrative databases. Linear regression was used to test the association between mental fatigability (PFS) as the dependent variable and patients’ nadir Hb as the primary predictor variable controlling for age, gender, race, ethnicity, Charlson Comorbidity Index, sickle cell anemia, history of depression, and physical fatigue level (measured by the PROMIS-SF8).
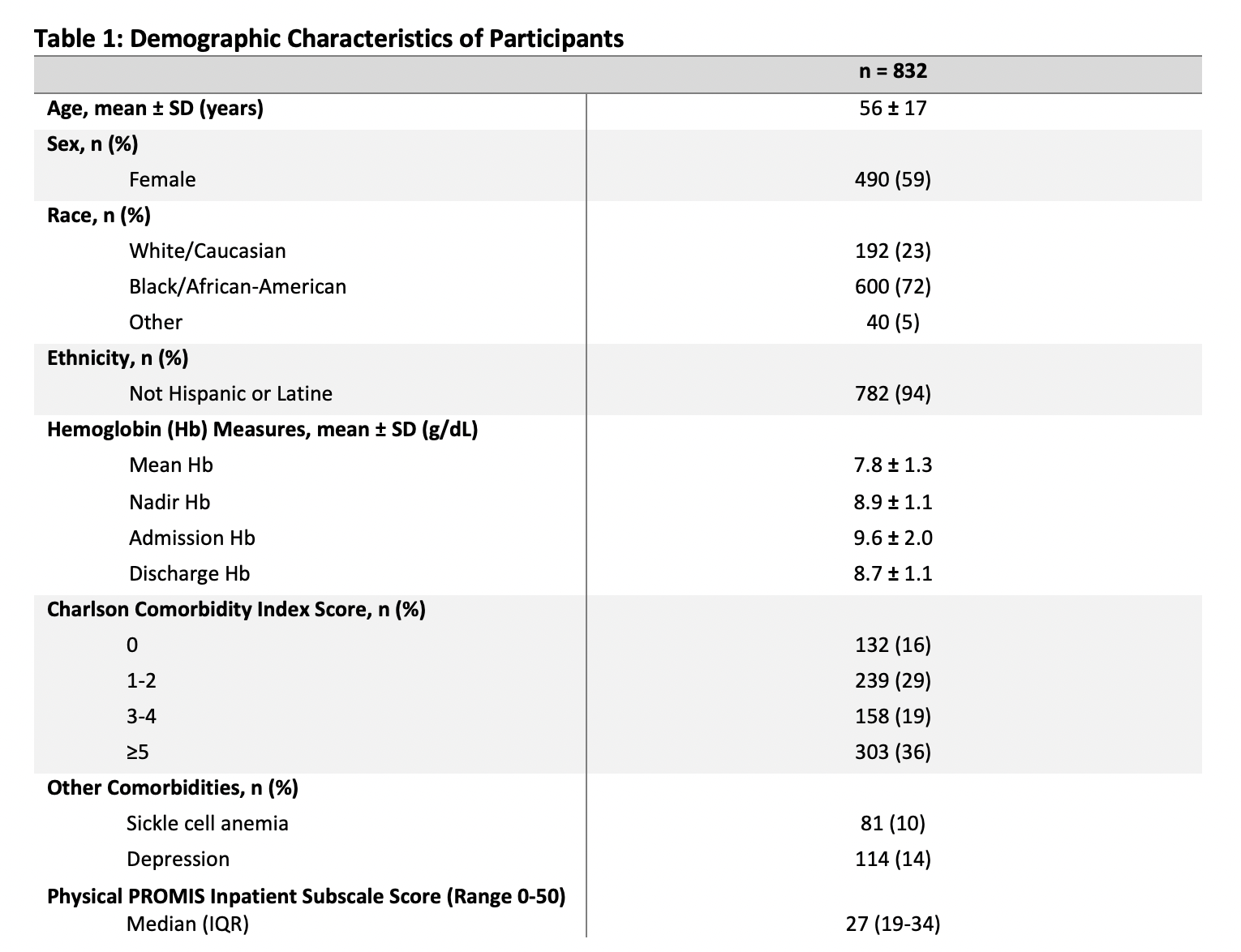
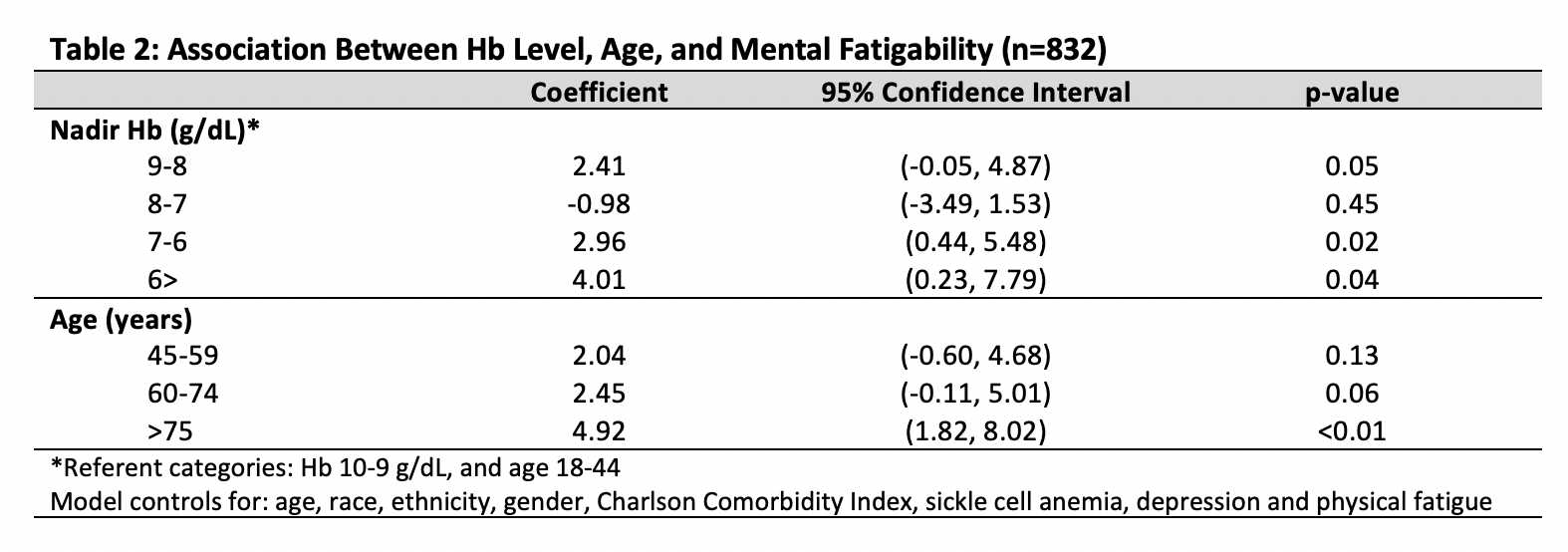
Results: A total of 832 patients had a Hb< 10g/dL and completed the inpatient mental fatigability questionnaire (Table 1). The average age was 56, 59% were female, and 72% were African American. The median nadir Hb level was 8.9g/dl. In the regression model, a lower nadir Hb was associated with increased mental fatigability, with patients’ having greater mental fatigability levels within each decreasing Hb strata except for Hb 7-8g/dL, compared to patients whose Hb was between 9-10g/dL during their hospitalization (Hb: 8-9g/dL, β=2.4, p=0.05; Hb: 7-8g/dL, β=-0.98, p=0.45; Hb: 6-7g/dL, β=3.0, p=0.02; Hb< 6g/dL, β=4.0, p=0.04) (Table 2).
Conclusions: Lower Hb levels are associated with higher mental fatigability levels, suggesting that hospitalized patients with anemia are at high risk for increased mental fatigability. While future work should focus on the mechanisms of mental fatigability and identifying mitigation strategies, hospitalists should be aware that patients with anemia are at increased risk of decreased activity levels and reduced cognitive functioning as a result of increased mental fatigability.