Background: The Limited English Proficiency (LEP) population is at higher risk of receiving poorer care and worse health outcomes compared to their English-speaking counterparts. Interpreters should be utilized to help improve these encounters, but physicians are rarely trained on how to work with interpreters effectively. This is reflected in a prior study showing that residents reported a lack of self-efficacy in their ability to deliver care to LEP patients. An online survey consisting of open and closed questions was sent to all pediatric residents (n=53) at a tertiary freestanding children’s hospital to capture perceptions on encounters that require an interpreter. We found that most survey responders were frustrated with encounters requiring interpreters. Purpose: To improve the interpreter-physician dynamic by having interpreters train residents on how to utilize language services to decrease frustration and increase comfort during LEP patient encounters. This will facilitate better communication and an increased understanding of the roles between the physician and interpreter with the overall goal of improving patient care and health equity.
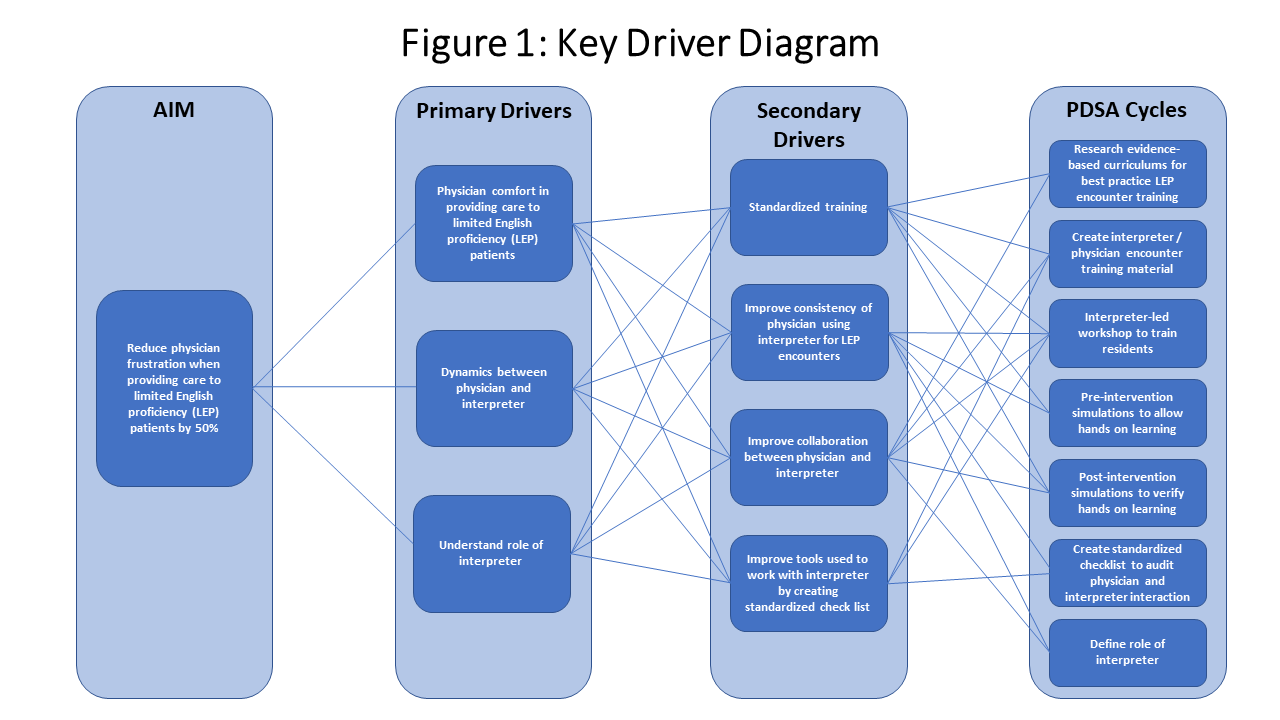
Methods: We approached this project using quality improvement tools (Figure 1). Additionally, 10 pediatric residents participated in an objective structured clinical exam (OSCE) that focused on communication skills. We scored them on a ‘yes/no’ 16-point observation checklist to gather baseline data. Afterward, a workshop was created to train the residents on how to partner with language services to facilitate these encounters. The workshop included (a) a lecture on proper utilization, (b) hands-on training through simulated patient scenarios, and(c) one-on-one time with certified interpreters to learn about their role. After completing the workshop, post-intervention data was collected on the same 10 pediatric residents using the same 16-point checklist and all residents in attendance received the online survey again. Descriptive statistics were performed to determine the outcomes on the online survey, and paired t-test was done to determine the difference between the pre- and post-intervention OSCE.
Results: The initial online survey had a 56.6% (n=28) response rate with 96.4% (n=27) stating that they felt frustrated when providing care for LEP patients; 77.8% (n=21) attributing it to language barriers. From the 10 pediatric residents who completed the pre- and post-intervention OSCE, the mean score increased from 10.1 to 13.7 (p-value = 0.002). 85% (n=34) of residents who attended the workshop (n=40) graded the workshop as good or excellent, and 82.5% (n=33) stated that they would change their current practice regarding LEP patients. The percentage of residents who rated their level of comfort in providing care to LEP patients as “comfortable” or “very comfortable” increased to 77% from 64%.
Conclusions: This study shows that this intervention is a feasible way to improve physician comfort and teach residents the skills needed to partner with language services to provide better care to LEP patients. This project is reproducible and can be modified to fit the needs of other departments and/or residency programs.