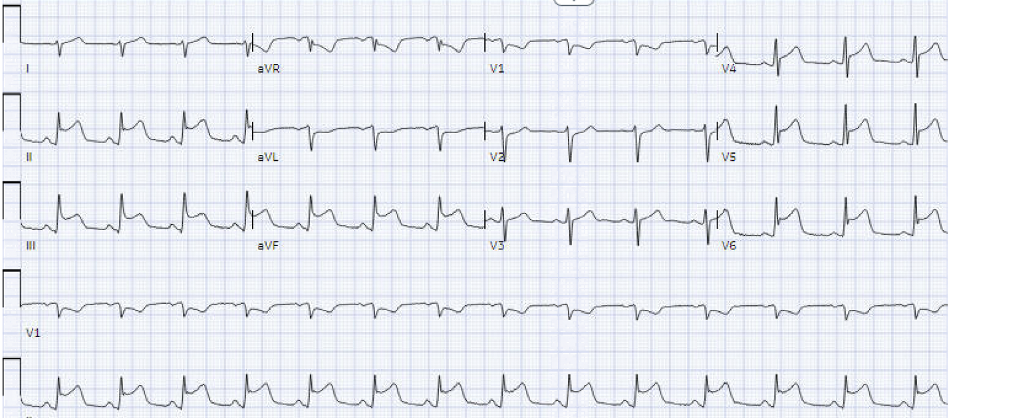
Case Presentation: A healthy 43-year-old Caucasian male who recently traveled to East Africa was presented to the emergency department with a high-grade fever (105.3F), and myalgia. He denied taking malaria chemoprophylaxis. On presentation, he was febrile, hypotensive, and tachycardic. He appeared to be ill, and toxic with no palpable organomegaly. His initial blood tests revealed leukopenia, thrombocytopenia, elevated serum creatinine, elevated bilirubin, and anion gap metabolic acidosis. Chest X-ray was unremarkable. The parasite smear returned with 9.4% parasitemia favoring Plasmodium falciparum. He was treated with artesunate for severe malaria. On day 2, he reported chest discomfort, which was aggravated by inspiration, and alleviated by leaning forward. High sensitivity Troponin I was elevated and peaked at >22,000. EKG showed diffuse ST elevation in II, Ill, aVF, and V4-V6. ST changes were normalized in serial EKGS. Echocardiogram showed left ventricular ejection fraction (LVEF) of 40% with moderate global hypokinesia. The parasitemia peaked at 39.4%. He was unable to undergo ischemic evaluation, cardiac MRI, or endomyocardial biopsy in the setting of hemodynamic instability and severe thrombocytopenia. A diagnosis of malaria myocarditis was made based on clinical suspicion. He was treated with 5 days course of artesunate and supportive management for malaria myocarditis. He was hospitalized for more than 5 weeks with severe malaria complicated by myocarditis, ARDS, renal failure, and liver failure. Fortunately, after the prolonged course of his hospital stay, he was stable to be discharged.
Discussion: Malaria is a mosquito-borne illness caused by a parasite. In 2020, an estimated 241 million cases of malaria occurred worldwide, and among them, 627,000 died according to the CDC. Plasmodium falciparum is well-known for its fatal complications such as cerebral malaria, shock, acute respiratory distress syndrome (ARDS), renal failure, and liver failure. However, cardiac complications such as myocarditis have been rarely reported to our knowledge. Historically, the heart was believed to be frequently injured in severe malaria involving up to 14% of fatal cases. The pathophysiology of cardiac involvement in severe malaria is still unclear. Fortunately, our patient survived after suffering devastating severe malaria due to Plasmodium falciparum. Our case highlights the importance of pre-travel advice and adequate chemoprophvlaxis in non-immune travelers.
Conclusions: Physicians should be aware of cardiac involvement in severe malaria. It is very important to educate patients on the importance of chemoprophylaxis along with barrier protection such as insect repellent and insecticide-treated bed netting to prevent life-threatening malaria.