Background:
Community‐acquired pneumonia (CAP) is the most common infectious cause of death in the United States and has thus been the target of numerous quality initiatives. Early administration of guideline‐concordant antibiotics, influenza and pneumo‐coccal vaccination, and obtaining blood cultures have been shown to decrease mortality in CAP. However, the impact of their greater use on the outcomes of CAP patients over time has not been demonstrated. We examined the trend in mortality of patients hospitalized with CAP.
Methods:
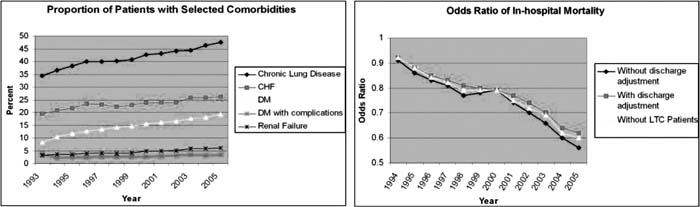
Our analysis used hospitalizations from a 10% subsample of the Healthcare Cost and Utilization Project National Inpatient Sample from 1993 to 2005. Cases of CAP in patients ≥ 18 years were identified by a principle diagnosis of pneumonia or respiratory distress/failure with a secondary diagnosis of pneumonia (shown to have a sensitivity of 84% and specificity of 86%). Using the AHRQ Comorbidity Software, 29 binary comorbidity indicator variables (CIVs) were defined based on the secondary diagnoses coded at discharge. Univariate logistic regressions of inpatient mortality on each CIV were performed separately. Only the 25 that predicted an increased mortality risk were used subsequently because a decreased risk likely indicates coding bias. A multivariate logistic regression was then performed, regressing mortality on the following independent variables: dummy variables for each year (reference year 1993), age by 5‐year category, sex, and the 25 CIVs. The primary outcome measure was the odds ratio (OR) of death in each year relative to 1993. To adjust for changing admission and discharge practices, the regression was repeated, excluding patients admitted from long‐term care facilities and, separately, including dummy variables for discharge to a skilled nursing facility (SNF), intermediate care facility (ICF), or with home health care. To assess the sensitivity of our results to increases over time in the number of fields available for coding (and a consequent increase in the proportion of patients with CIVs), we repeated the multivariate regression after restricting all patients to a maximum of 5 discharge diagnoses.
Results:
In total, 389,639 patients met the coding criteria, most of whom were in their fifties (11%), sixties (16%), seventies (24%), and eighties (23%). Over the period studied, mean length of stay declined from 8 to 5.5 days, whereas the percentage of patients discharged to a SNF/ICF and with home health care increased from 15% to 22% and from 5% to 12%, respectively. Mortality adjusted only for age and sex declined from 9% to 5.7%. Figure 2 shows the OR of multivariate‐adjusted mortality in each year relative to 1993, with an OR of .56 (.51‐60) in 2005. After restricting all patients to a maximum of 5 diagnoses, this OR was .59.
Conclusions:
The prevalence of comorbidities in hospitalized CAP patients has increased, whereas mortality has been greatly reduced. Continued efforts to increase use of the aforementioned beneficial interventions may further reduce mortality in CAP.
Author Disclosure:
G. W. Ruhnke, none.