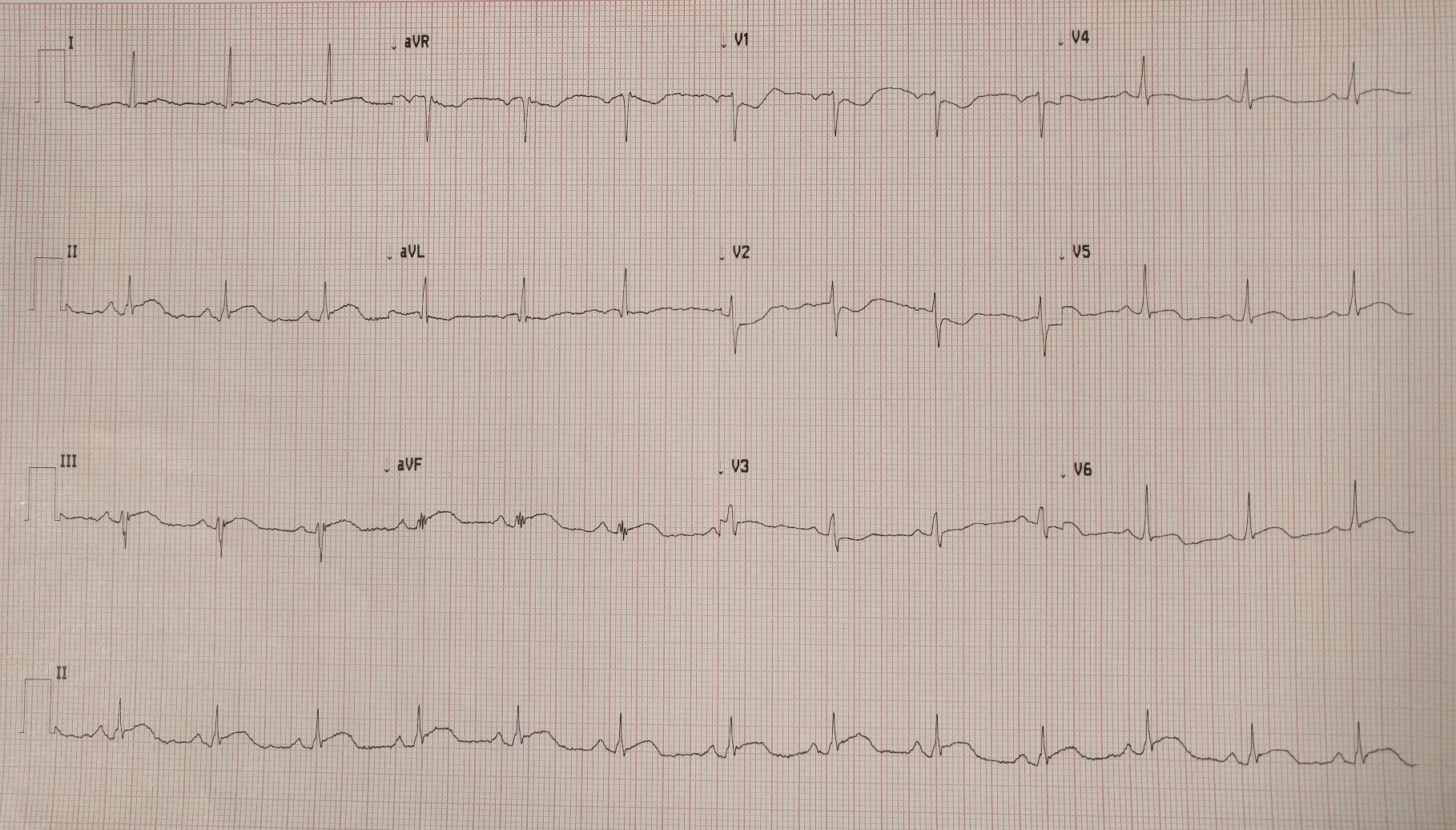
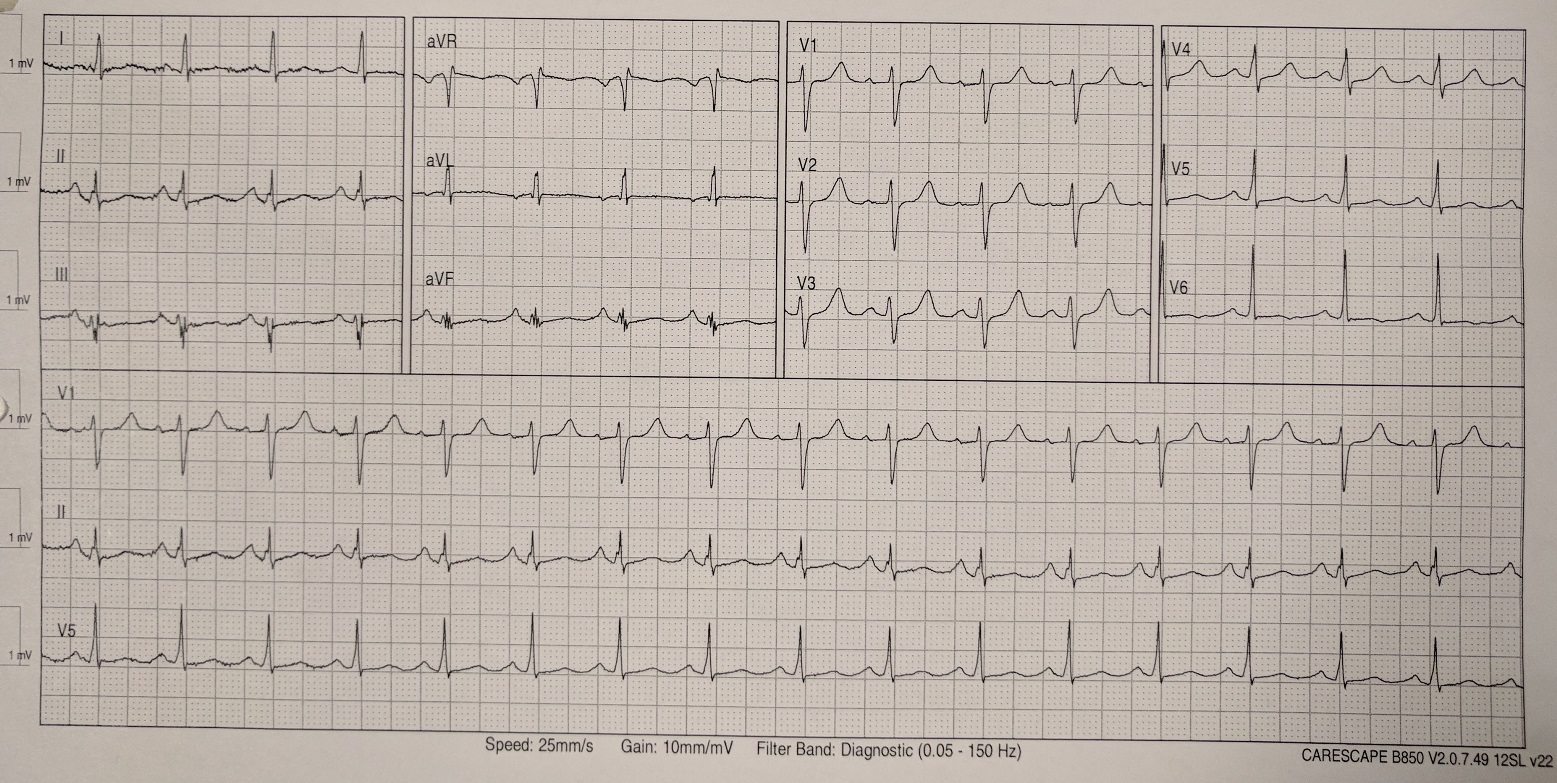
Case Presentation: A 54-year-old female with no significant past medical history presented with lip swelling and shortness of breath following shellfish ingestion. She denied chest pain. Due to concern for angioedema, she received intramuscular epinephrine, intravenous methylprednisolone, diphenhydramine and famotidine. A 12-lead electrocardiogram revealed 2 mm ST segment elevation in leads II, III and aVF (Figure 1). Troponin I level was normal at 0.020 ng/ml (reference range: 0.000 – 0.045 ng/ml). Coronary angiography via cardiac catheterization revealed normal coronary arteries. Six hours following initial presentation, repeat electrocardiogram revealed complete resolution of the ST segment elevations (Figure 2) and troponin I level peaked at 8.330 ng/ml. Her acute presentation was most likely due to coronary artery vasospasm secondary to an acute hypersensitivity reaction to shellfish. She was started on amlodipine for coronary artery vasodilatation.
Discussion: Kounis syndrome (KS) is not uncommon, but it is infrequently recognized and diagnosed. Several environmental, food and drug exposures have been described to trigger KS, including shellfish, canned food and non-steroidal anti-inflammatory drugs.Three different types of KS have been described in the literature. Type I manifests as coronary artery vasospasm in patients with normal coronary arteries. Our patient’s presentation is most consistent with this type. Type II KS is seen in patients with preexisting atheromatous plaques that erode, rupture and form thrombi after an acute hypersensitivity reaction. Type III KS manifests as coronary artery stent thrombosis following an acute hypersensitivity reaction. In addition to coronary artery involvement, KS can cause ischemia or infarction in other arterial systems such as the mesenteric and cerebral arteries.KS results from mast cell degranulation following an acute hypersensitivity reaction. This leads to the release of inflammatory mediators including histamine, chymase, platelet-activating factor and leukotrienes. These mediators are directly implicated in coronary artery vasospasm and atheromatous plaque rupture. Diagnosis is based on the clinical presentation supplemented by laboratory, electrocardiographic and angiographic findings.Treatment of KS consists of first aborting the acute hypersensitivity reaction and then stabilizing the coronary vasculature with standard medical and interventional techniques. Initial management should include the use of epinephrine, corticosteroids and antihistamines to reduce the transcription of pro-inflammatory cytokines. This improves coronary artery vasospasm in type I KS and reduces the downstream cytokine effect on unstable coronary artery plaques in type II KS. This should be followed by standard acute coronary syndrome medical therapy. For type I KS, coronary artery vasodilators such as nitrates and calcium channel blockers are helpful. Beta-blockers may potentiate coronary artery vasospasm if used acutely by causing unopposed alpha-adrenergic receptor stimulation.
Conclusions: KS is a complex condition that may manifest in individuals with acute hypersensitivity reactions. Awareness of both the cardiac and anaphylactic pathophysiology is important as diagnosis and treatment can be challenging. Clinicians should keep the diagnosis in mind when assessing patients with acute allergic symptoms. More literature about KS is required to improve prevention and treatment.