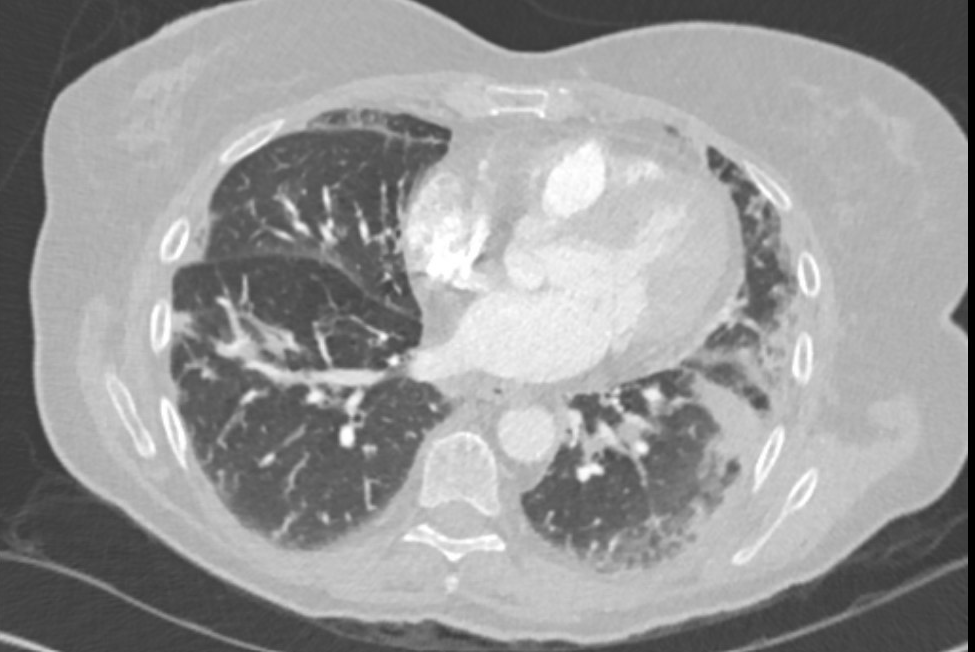
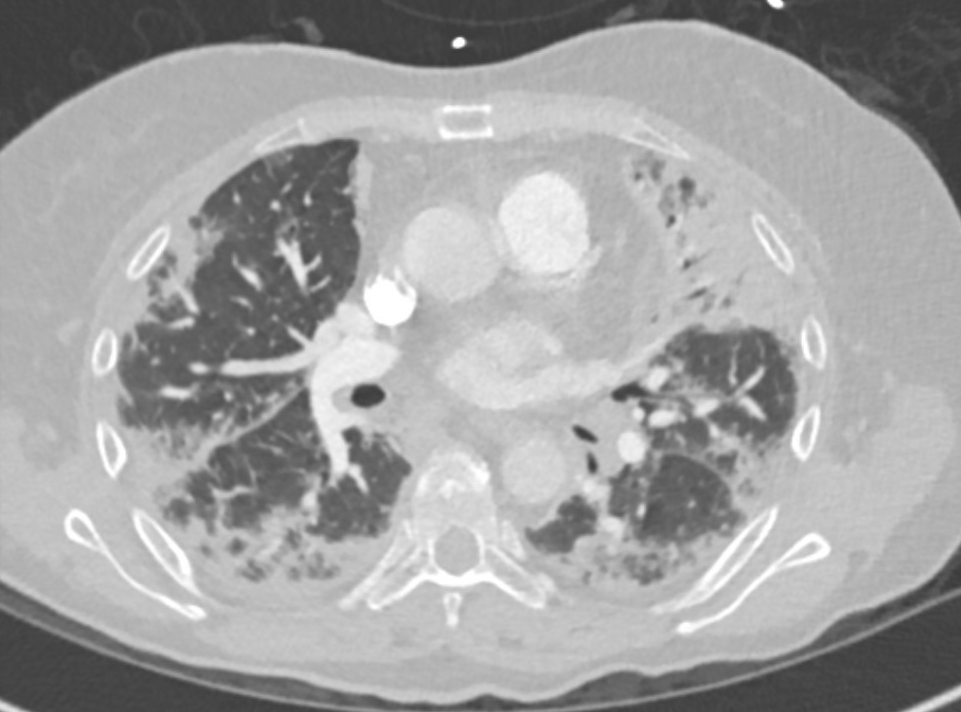
Case Presentation: A 65-year-old female with a past medical history of hypertension, hyperlipidemia, coronary artery disease, and tobacco abuse was admitted to the hospital for worsening shortness of breath and cough. The patient was initially admitted to the hospital for cough and shortness of breath. CT chest revealed multifocal pneumonia and the patient was started on IV antibiotics. The patient was hypoxic on room air and required supplemental oxygen. During the hospital stay, there was an apparent improvement in the patient’s symptoms and the patient was discharged home on oral antibiotic and home oxygen. However two weeks after hospital discharge patient presented to ED again with worsening shortness of breath and cough. CT chest showed worsening bilateral pulmonary opacities which raised concern for COVID pneumonia as well as multifocal pneumonia vs other inflammatory pulmonary processes. COVID test was done twice and resulted in negative. The patient was started on pulse dose IV solumedrol. Initial rheumatology workup came back negative. However, the patient’s respiratory symptoms continued to worsen requiring BiPAP followed by intubation within a short period of time. Later on, the patient was noted to have faint rash over knuckles that raised suspicion for Gottron’s papule. A diagnosis of MDA5 Dermatomyositis (DM) with Rapidly Progressive Interstitial Lung Disease (RP- ILD) was suspected. A myositis panel was sent and the patient was started on IV Tocilizumab. However, the patient’s respiratory status continued to worsen rapidly and she ultimately expired. Later on, the result of myositis specific 11 Ab panel came back positive for high titer of MDA-5 Ab >100.
Discussion: Dermatomyositis (DM) is a disease entity that presents with classic skin rashes as well as the involvement of skeletal muscle. It has various forms of disease spectrum and anti-melanoma differentiation-associated gene 5 (MDA5) DM is the most recent form which usually presents with rapidly progressive (RP) Interstitial Lung Disease (ILD). MDA5 dermatomyositis is also typically associated with various skin manifestations like skin and oral ulcerations, and painful palmar papules and macules. RP ILD in MDA5 dermatomyositis is often fatal with high early mortality. Patients with RP ILD have a poor response to treatment. Due to predominant lung involvement, this clinical presentation may be confused with differentials like bacterial pneumonia, COVID-19 pneumonia, and hypersensitivity pneumonitis. Anti-MDA5 Ab is positive in MDA 5 dermatomyositis. Due to its high mortality, early diagnosis of the disease is crucial so that early and aggressive treatment with immunosuppressive drugs can be initiated.
Conclusions: This case highlights the importance to keep a high index of suspicion for MDA5 dermatomyositis in a patient with rapidly progressive and worsening hypoxia and skin rash with bilateral pulmonary opacities. So that early diagnosis and initiation of immunosuppressive drugs can be done in time.