Background: In 2010, the Patient Protection and Affordable Care Act (ACA) aimed to enhance health insurance access through subsidies and Medicaid expansion. The expansion was not adopted by all states, leading to variable coverage. The Centers for Medicare & Medicaid Services (CMS) releases a 3-year running average of 30-day risk-standardized mortality rates for Medicare patients with heart failure (HF) discharged from all acute care hospitals nationwide. Post-hospital discharge mortality highlights issues of access and care planning. States expanding Medicaid may observe reduced mortality rates compared to non-expanding states. To test this, we analyzed the national 30-day post-discharge mortality rate after HF admission since 2005, assessing whether hospital mortality rates differ based on the Medicaid expansion status of their respective states.
Methods: We obtained data from four sources: 1) hospital characteristics and risk-standardized 30-day mortality rate data from CMS, 2) regional demographic and economic data from the US Census Bureau, 3) ZIP code mapping to hospital catchment area data from the Dartmouth Atlas of Healthcare, and 4) year when states allowed Medicaid expansion from the Kaiser Family Foundation. We categorized states into those expanding Medicaid by 2014 and those not expanding until 2020, excluding five states that expanded between 2014 and 2020. Data were summarized using mean (SD) or percentages, and differences were analyzed with the Chi-square test or Wilcoxon rank-sum test. Examining the relationship between Medicaid expansion and 30-day mortality post-HF hospitalizations utilized a difference-in-difference framework with multilevel models. Adjusted models included confounding variables such as hospital ownership, teaching status, number of beds and nurses, rural/urban location, and catchment area demographics (total population, median income, poverty percentage, African American percentage, and insurance percentage).
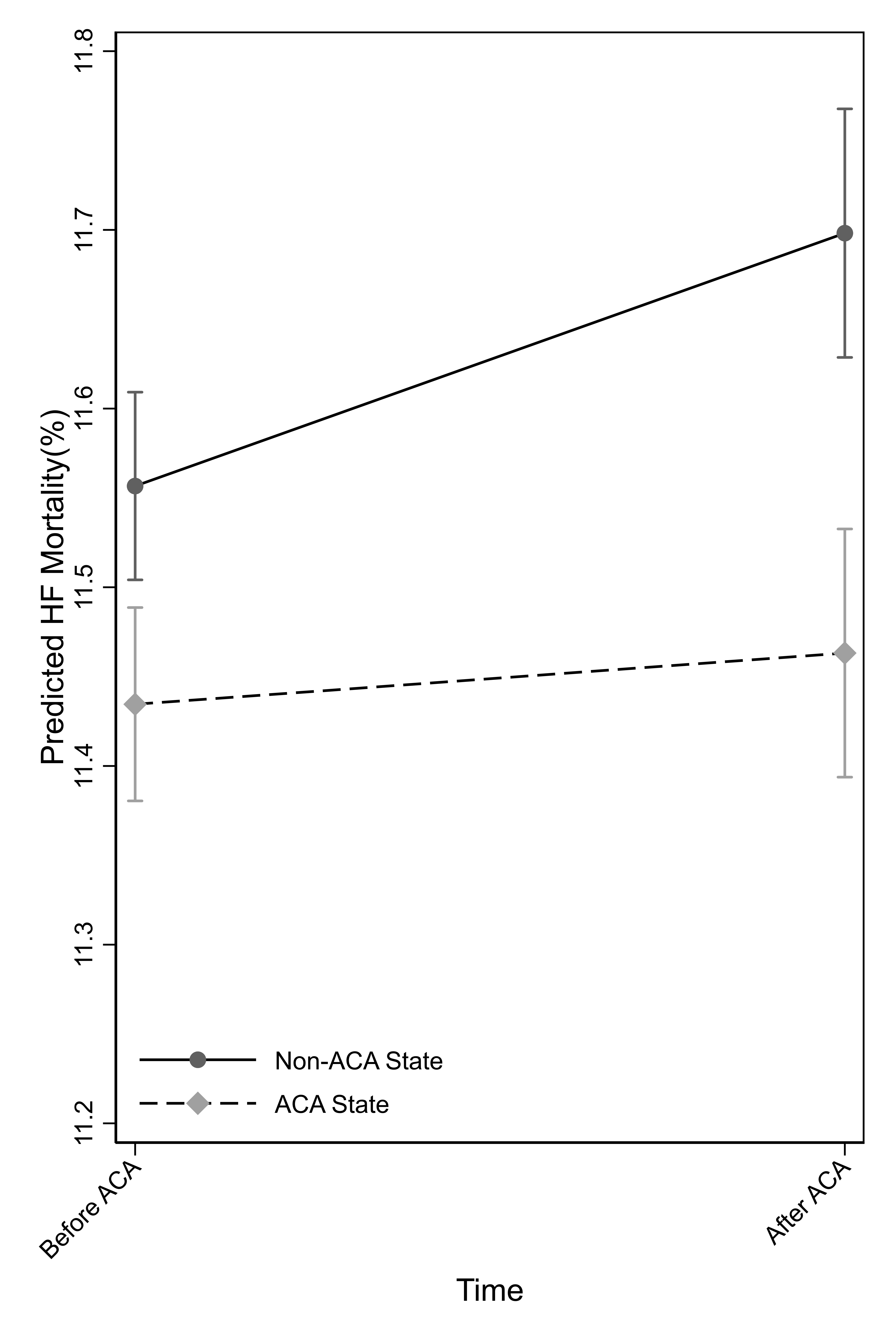
Results: Of the 3,839 hospitals, 52% (2,012) were in Medicaid expansion states (N=26). States without Medicaid expansion (N=19) had more for-profit hospitals (21% vs. 10%; P< 0.001), rural hospitals (47% vs. 36%; P< 0.001), and non-teaching hospitals (84% vs. 70%; P< 0.001). Before 2014, 30-day mortality rates were higher in hospitals from the non-Medicaid-expansion states than from Medicaid-expansion states (HF = 11.6% vs. 11.4%; P< 0.001). Hospitals located in non-Medicaid expansion states had a significant increase in mortality rate after 2014 than before 2014 (difference = 0.11%, 95%CI = 0.05% to 0.18%; P=0.001). In contrast, the mortality rate did not change in hospitals located in Medicaid-expansion states (difference = 0.01%, 95%CI =-0.07, 0.08; P=0.85). However, there was a significant difference in the time trend between the Medicaid-expansion states and non-Medicaid expansion states (difference-in-difference: -0.11%, 95%CI = -0.20 to -0.02%; P=0.02). These results remained significant after adjusting for hospital and regional population characteristics (difference-in-difference: -0.11%, 95%CI = 0.21%, -0.02; p=0.02) (Figure 1).
Conclusions: Post-ACA, Medicaid-expansion state hospitals showed stable 30-day post-discharge mortality rates for heart failure, contrasting with significant increases in non-expansion states. Improved healthcare access from Medicaid expansion likely contributed to this difference.