Background: Medical misadventure, defined as unintended harm caused during medical care or procedures, is an increasingly significant concern in patient safety and healthcare quality. Recent decades have seen heightened awareness and reporting of such incidents globally, including in the United States. This study quantifies trends in medical misadventure-related mortality and morbidity by examining regional disparities within the U.S., highlighting the shifts in burden over the past two decades. By analyzing these patterns, the research aims to provide insights into systemic factors contributing to these adverse events and to inform strategies for prevention and quality improvement in healthcare delivery.
Methods: Analysis of medical misadventure-related deaths in the US from 1999-2020 was conducted for adults aged 25 and older using death certificate data from the CDC WONDER database, utilizing the ICD-10 code Y60-69. Age-adjusted mortality rates (AAMR) per 1,000,000 population were extracted, and trends were analyzed using Joinpoint regression to calculate the Average Annual Percent Change (AAPC) with p value for statistical significance. Data were stratified using year, gender, race/ethnicity and geographical regions.
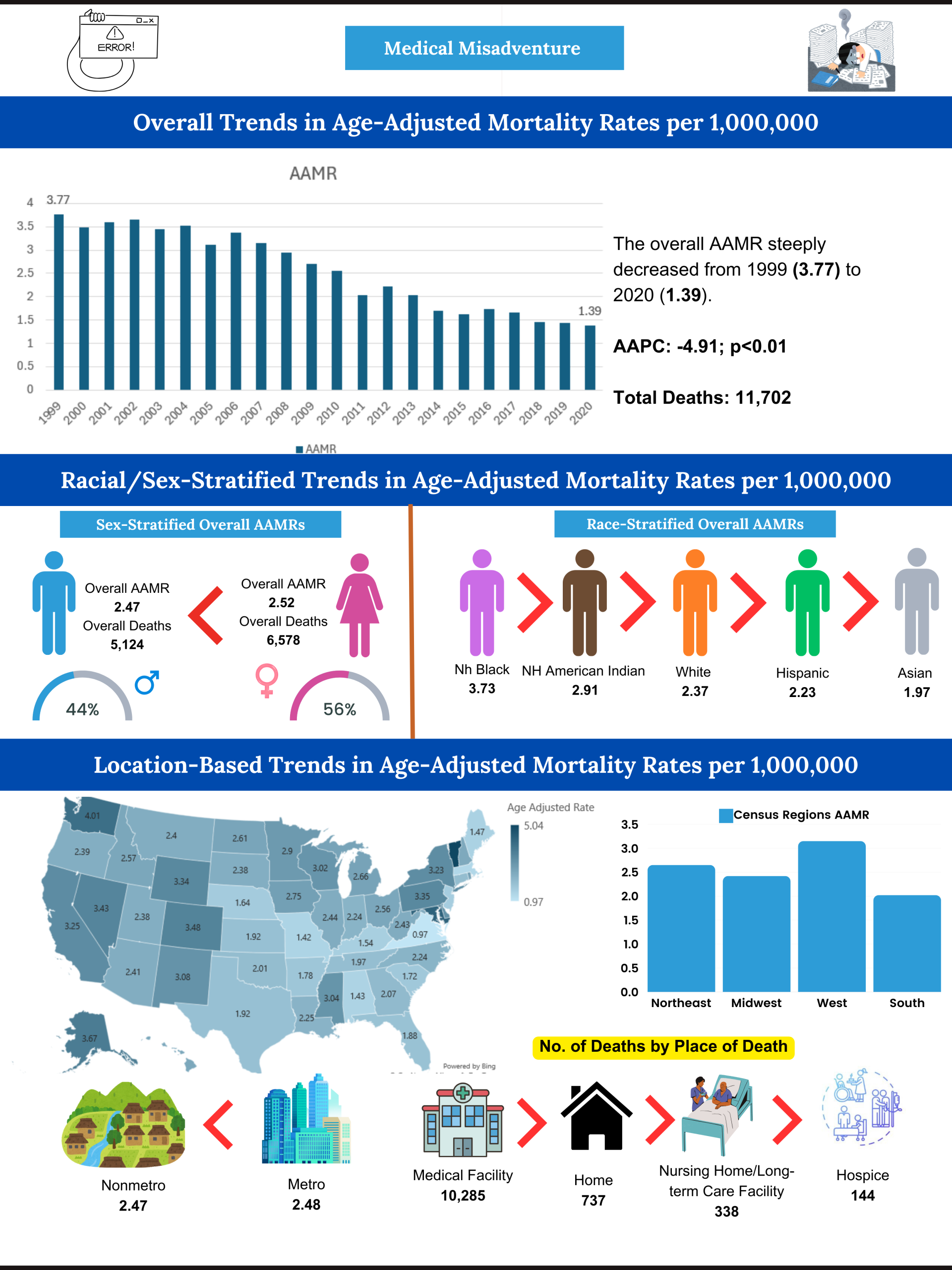
Results: Between 1999 and 2020, medical misadventure accounted for 11,702 deaths among U.S. adults aged ≥25 years. Most deaths occurred in medical facilities (87.9%) followed by decedents homes (6.3%). The overall AAMR for medical misadventure-related deaths decreased from 3.77 in 1999 to 1.39 in 2020, with an AAPC of -4.91 (p< 0.01). Women showed higher AAMRs than men (2.52 vs. 2.47), with a more pronounced decrease in men (AAPC: -5.15 , p< 0.01), compared to women (AAPC: -4.46 , p< 0.01). Racial disparities were significant, with NH Black having the highest AAMR (3.73), followed by NH American Indian (2.91), NH White (2.37), Hispanic (2.23), and NH Asians or Pacific Islanders (1.97). The decline in AAMR throughout the study was most pronounced in Hispanics (AAPC: -6.61, p< 0.01). Geographically, the highest AAMRs were observed in Vermont (5.04) and the lowest in Virginia (0.97). Western U.S. had the highest regional AAMR (3.15), followed by the Northeast (2.65), Midwest (2.42), and South (2.02). Metropolitan areas had higher AAMRs than nonmetropolitan areas (2.48 vs 2.47), though metropolitan areas showed steeper decline from 1999 to 2020 (metropolitan: AAPC: -5.17, p< 0.01).
Conclusions: Uniform decrease in mortality was seen, however, demographic and regional disparities persist in medical misadventure-related mortality. These findings emphasize that overtime mortality has significantly fallen which shows an improvement in the decision making of physicians and care provided by the medical staff.