Background: The concept of using Entrustable Professional Activities (EPAs) in undergraduate medical education (UME) arose because residency program directors noticed a significant decline in their interns’ ability to perform the basic skills required of them upon starting residency. The internal medicine (IM) sub-internship (sub-I) rotation is primed to address the EPAs especially pertinent to the hospitalized patient. Accordingly, we created a high fidelity simulation curriculum to both teach and evaluate a student’s ability to recognize and stabilize decompensating patients (EPA 10) and to assess teamwork skills (EPA 9). Sutaria et al found that individual simulation may be better suited for EPA evaluation of students than group simulation. However, the student experience of group compared to individual simulation is unknown.
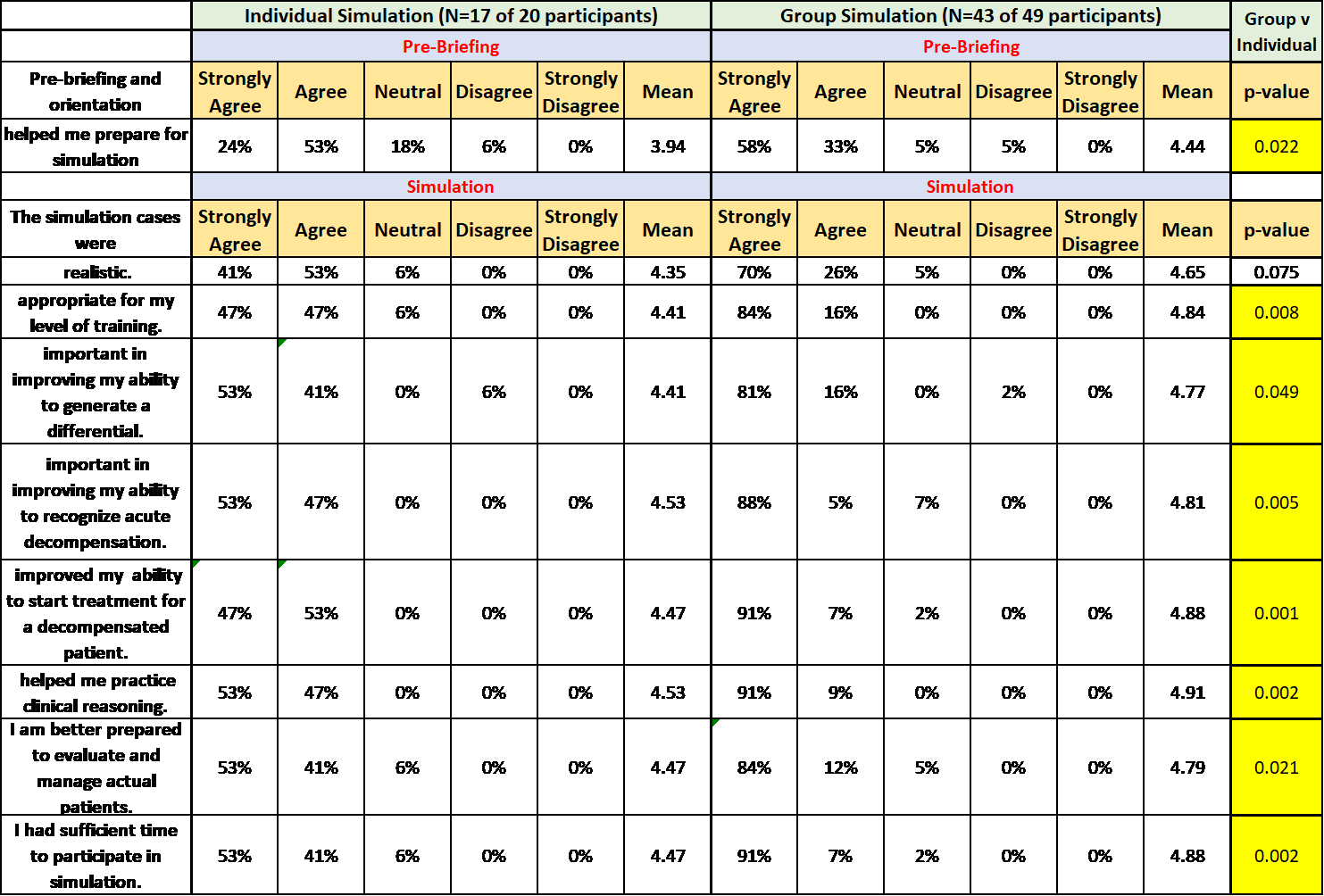
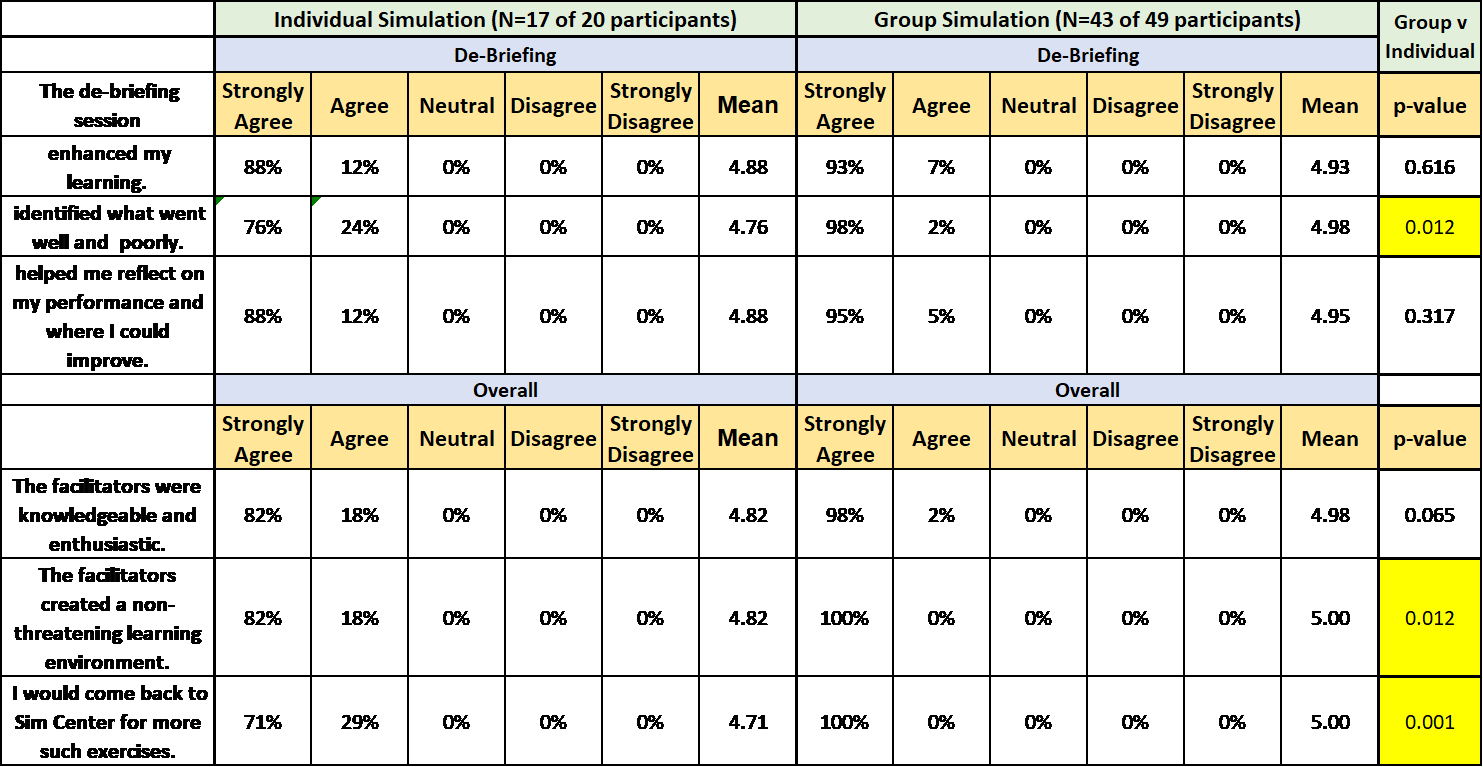
Methods: Simulation certified hospital medicine faculty developed a simulation curriculum for the IM sub-I rotation involving 5 high fidelity patient scenarios (acute upper GI bleed, community acquired pneumonia, diabetic ketoacidosis, acute coronary syndrome and pulmonary embolism) to assess student performance on EPAs 9 and 10 and to provide targeted feedback and teaching during de-briefing. A total of 69 students (N=49 in group and N=20 in individual) participated in the simulation curriculum. All went through pre-brief, simulation and de-brief. Group simulation students performed 4 different cases. Each of the students took a turn as team lead. Individual simulation students performed 1 case. Gaps in evaluation and treatment during simulation were noted and specifically addressed during de-briefing.Course evaluations asked students to evaluate the efficacy of pre-briefing, simulation and de-briefing on a 5-point Likert scale (strongly agree to strongly disagree). Fisher’s exact analysis was performed to compare students who strongly agreed to each survey question. A p-value of <0.05 was considered significant.
Results: 60 of 69 students completed the evaluation for an 86.9 % response rate [individual N=17/19 (85%), group N= 43/50 (87%) p=NS]. Overall, the course was very highly rated by both groups (Table 1). The de-briefing was the highest rated component (Table 2). 91% of sub-Is in group simulation strongly agreed that the simulation cases were important in improving their ability to initiate urgent treatment for a decompensating patient compared to only 47% of students who performed individual simulation (p=0.001). In the group simulation, more students strongly agreed that simulation faculty were knowledgeable enthusiastic and created a non-threatening learning environment (98%) compared to individual simulation students (82%) p= 0.012. 100% of the group simulation students strongly agreed that they would return for more similar, simulation sessions compared to only 71% of individual simulation students (p=0.001).
Conclusions: Incorporating high fidelity simulation exercises to the IM sub-internship was well received in both the group and individual formats. IM sub-Is rated group simulation higher than individual simulations. Due to the significant faculty time commitment needed for individual simulation, individual students only performed 1 case compared to the 4 cases done in group simulation. The time and resources needed for individual simulation may be best reserved for evaluation purposes. For teaching purposes, group simulation may be both preferred by students and better leverage faculty time.