Background: Survivors of hospitalization for COVID-19 are potentially at high risk for subsequent psychiatric morbidity due to medical trauma, systemic inflammation, and potential neurotropism of SARS-CoV-2(1). In addition, social isolation during the hospital stay due to restrictive visitor policies and after discharge due to fears of contagion or stay-at-home orders could further increase psychiatric vulnerability in all patients(2). Stay-at-home orders and delays of non-urgent treatment during the pandemic could also reduce the likelihood patients would seek or receive psychiatric treatment. Thus, we aimed to determine the prevalence of psychiatric symptoms among patients discharged from the hospital during the COVID-19 pandemic, and the relationship of COVID-19 diagnosis, isolation, and in-hospital psychological distress with post-hospitalization psychiatric symptoms.
Methods: Prospective cohort study in which patients who were discharged from a large academic medical center during the height of the 2020 COVID-19 pandemic in Michigan (discharge dates 4/4/2020-6/16/2020) were surveyed 30 to 40 days post discharge. Survey items included post-hospitalization symptoms of depression, generalized anxiety, post-traumatic stress, and loneliness measured using standard questionnaires (Patient Health Questionnaire-9 [PHQ-9], Generalized Anxiety Disorder-7 [GAD-7], Post-Traumatic Stress Disorder (PTSD) Checklist-2 item version [PCL-2], and 2 items from the UCLA loneliness scale, respectively). Survey responses were compared between COVID-positive and COVID-negative patients with additional assessments stratified by social isolation factors and in-hospital psychological distress. Generalized linear models were used to assess the association between COVID-19 diagnosis and psychiatric outcomes after controlling for age, sex, pre-existing conditions, length of stay, intensive care hospitalization, and isolation after discharge.
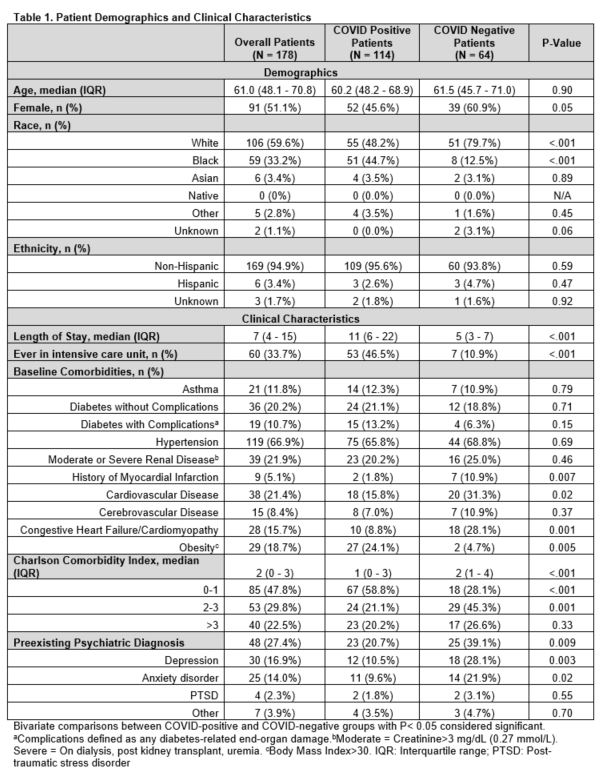
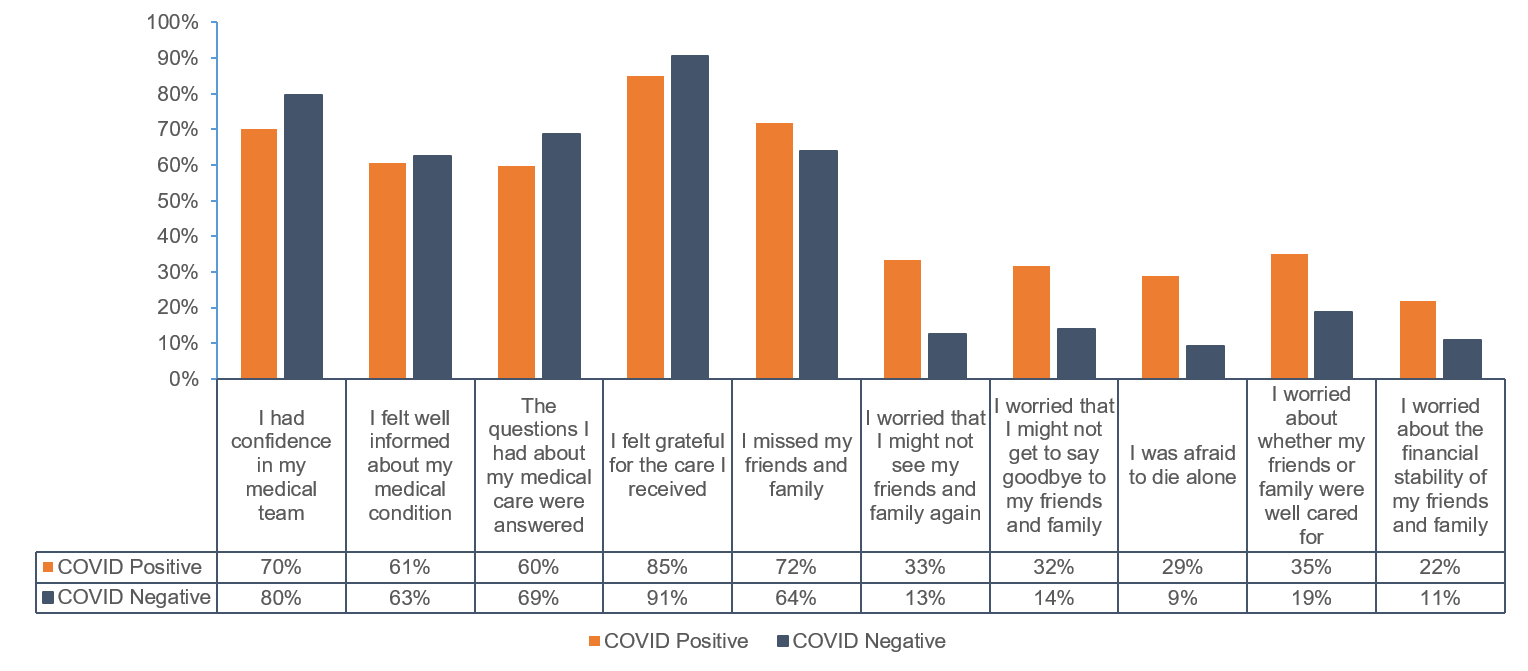
Results: Of 430 patients with attempted contact, 14 were excluded and 178 completed the survey (response rate 41.8% [178/416]) of whom 114 were COVID-positive (see Table 1 for patient characteristics). Compared to patients without COVID-19, patients with COVID-19 scored similarly on the PHQ-9 (3.4 vs. 4.4, P=0.2) and GAD-7 (3.5 vs. 2.8, p= 0.3), but higher on the PCL-2 (3.0 vs. 2.3, P=0.002) and loneliness questions (3.0 vs. 2.5, P=0.004) despite lower reported pre-existing psychiatric diagnoses (21% [23/114] COVID-positive vs. 39% [25/64] COVID-negative, P=0.009). A quarter (25% [27/110]) of COVID-positive patients screened positive for PTSD (vs. 6.6% [4/64] without COVID-19, P=0.003). Patients with COVID-19 also recalled higher levels of isolation-related psychological distress during hospitalization (Figure 1). COVID-19 diagnosis was an independent predictor of symptoms of anxiety, PTSD, and loneliness (Parameter estimate [95% CI] for GAD-7: 1.95 [0.30-3.60], P=0.02; PCL-2: 0.83 [0.25-1.41], P=0.005; loneliness: 0.57 [0.15-0.99], P=0.008).
Conclusions: COVID-19 survivors reported high prevalence of in-hospital psychological distress and post-traumatic stress symptoms after hospitalization. COVID-19 survivors should be screened for PTSD at post-discharge follow up, and hospitals should enact strategies to mitigate psychological distress in hospitalized patients with COVID-19.