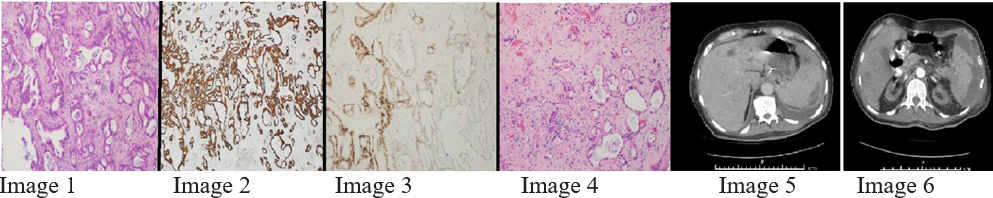
Case Presentation: A 78-year-old dialysis-dependent man with a history of end stage renal disease, hypertension and cerebrovascular accident was evaluated for diffuse abdominal pain and altered mental status for one day. The examination was pertinent for generalized weakness and altered sensorium. Laboratory tests revealed transaminitis and leukocytosis. Computed tomography (CT) of the abdomen and pelvis showed multiple hypoattenuating hepatic foci with hepatosplenomegaly. A set of blood cultures grew Clostridium inoculum. A pyogenic liver abscess was diagnosed, drained percutaneously and the culture grew pansensitive Escherichia coli. A follow up CT of the abdomen and pelvis revealed a large splenic abscess. Exploratory laparotomy, splenectomy, liver biopsy and peritoneal lavage were performed. Immunostaining of the sample was positive for CK7, CK20 and CDX2. Pancreaticobiliary adenocarcinoma metastatic to the spleen and liver was confirmed by pathology. CA 19-9 and CA 125 were elevated. A repeat CT of the abdomen with pancreatic protocol showed a pancreatic tail mass. Vancomycin resistant Enterococcus faecium grew on peritoneal fluid culture. Daptomycin and ceftriaxone were started. The patient improved clinically but he was deemed unsuitable for further invasive procedures or chemotherapy.
Discussion: Hepatosplenic abscesses presenting with pancreatic tail adenocarcinoma is rare and altogether heightens the diagnostic and therapeutic challenge. Pyogenic liver abscesses have been well-documented with an incidence of 1.85% in cancer patients while splenic abscesses are less associated in the literature. Uncommon presentations of pancreatic adenocarcinoma include gastrointestinal (GI) bleeding from metastasis and acute abdomen from splenic infarct. PLA is associated with GI malignancies including pancreatic cancer. Some experts recommend cancer evaluation for GI malignancies in patients with PLA. Mucosal barrier breach by cancer cells, translocation of bacteria into the circulation and inoculation at metastatic sites are possible explanations for developing liver and splenic abscesses. Dialysis is also a risk factor for hepatosplenic abscess. In an elderly patient with hepatosplenic abscess and elevated tumor markers, a thorough evaluation for GI malignancies including pancreatic cancer should be done. Pyogenic liver abscess may even be an indication of end stage hepatobiliary-pancreatic malignancy which correlates to a poor prognosis. Less than 20% patients are eligible for curative resection.
Conclusions: The diagnosis of metastatic pancreatic adenocarcinoma was elusive and only revealed after extensive investigation. This reminds physicians that an elderly patient with multiple hepatosplenic abscesses and elevated tumor markers must be thoroughly evaluated for underlying malignancy.