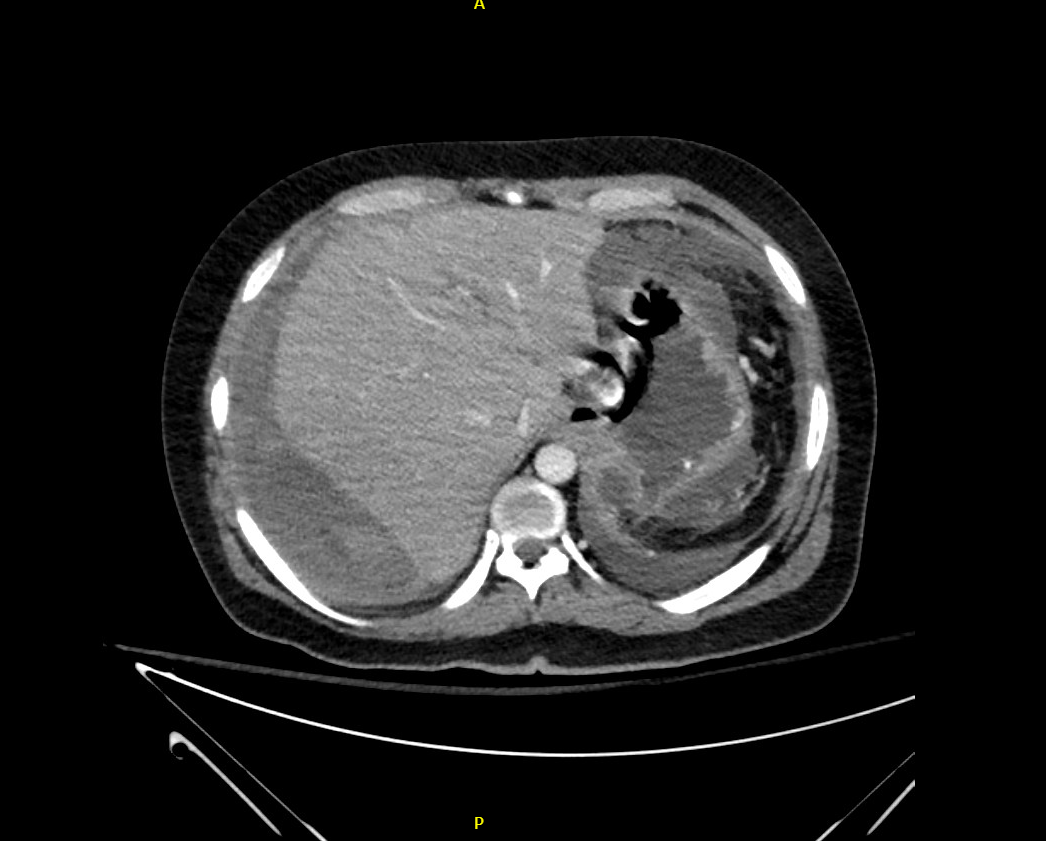
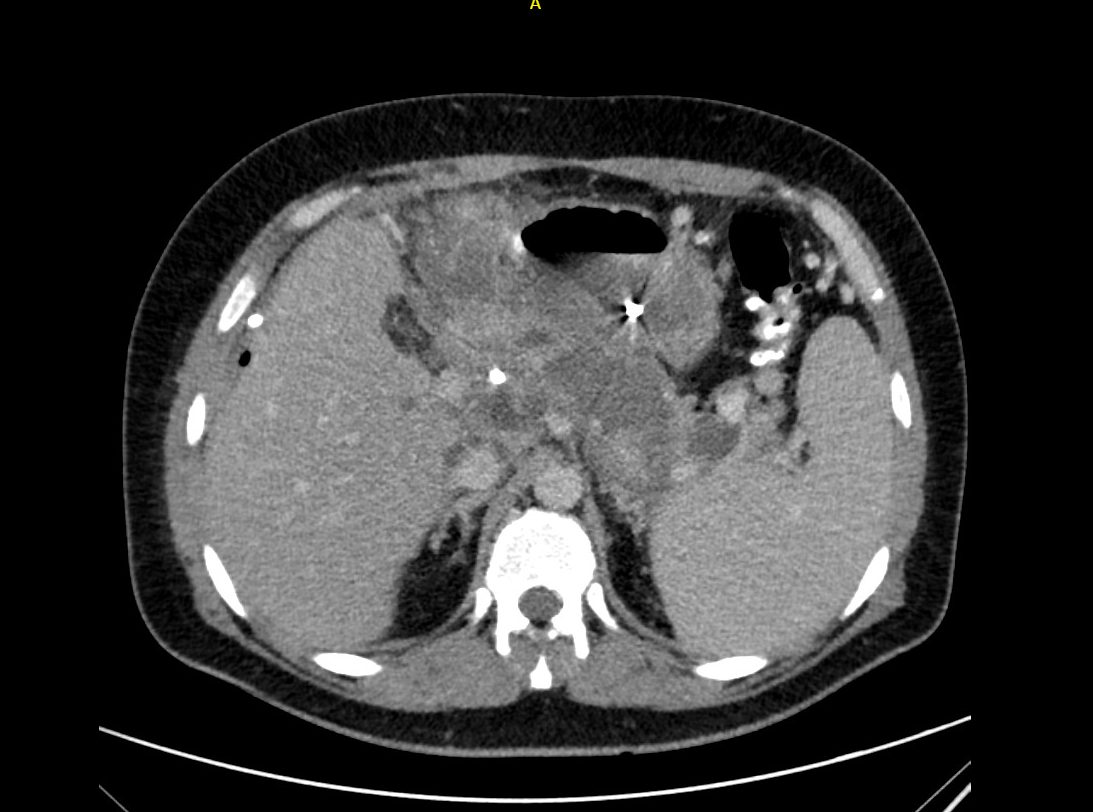
Case Presentation: A 36-year-old male with a PMH of alcohol use disorder, recurrent pancreatitis, cholecystectomy, diabetes mellitus type 2, and hyperlipidemia presented to the emergency room for severe epigastric abdominal pain, nausea, and vomiting for 2 days in the setting of heavy alcohol use prior to admission. Vital signs on admission were notable for hypertension. Laboratory workup was significant for lipase of approximately 4,000 U/L (ref. 73-350 U/L). A CT abdomen and pelvis demonstrated interstitial pancreatitis with gastric varices. BISAP score on admission was 0. Aggressive intravenous fluids and supportive care were initiated. During the hospital course patient developed hyperbilirubinemia suspected secondary to biliary obstruction. He ultimately underwent biliary drain placement after failed ERCP. Three days later he developed a fever prompting a repeat CT scan which demonstrated necrotizing pancreatitis with peripancreatic fluid collection. After one week he developed worsening pain at the site of the biliary catheter. CT abdomen and pelvis showed a 14.6 cm multiloculated fluid collection with active contrast extravasation concerning for hepatic hemorrhage. He had subsequent elevations of AST and ALT of greater than 20K U/L (ref. < 46 U/L) and 17K (ref. < 35 U/L), respectively, and creatinine of 2.05 mg/dL (ref. 0.6-1.30 mg/dL) from a baseline of 1.02 mg/dL consistent with acute liver and renal injury. He was intubated and transferred to the ICU. He subsequently underwent right hepatic artery branch embolization by interventional radiology. CRRT and N-acetylcysteine protocol were initiated. The patient was deemed not to be a liver transplant candidate. The patient was transitioned to comfort care measures and passed away surrounded by family members at bedside.
Discussion: Acute pancreatitis is an inflammatory process of the pancreas characterized by abdominal pain, nausea, vomiting, and an associated elevation of pancreatic enzymes in the blood. The reported annual incidence of acute pancreatitis is increasing worldwide [1,2]. Although the mortality rate is under 5 percent with the majority of patients suffering from mild disease, an average of 20% of patients have severe disease. This subset of patients are at higher risk multiorgan failure and death [3]. The patient described suffered a number of complications during his hospital course with hepatic artery hemorrhage ultimately resulting in death. While these complications vary in their rate of occurrence, severe bleeding is a relatively rare complication at a rate of 1.2-14.5% [7]. It is more often seen in necrotizing pancreatitis and results from direct erosion of an artery or pseudoaneurysm formation. The most common arteries involved are the left gastric and splenic arteries though the hepatic artery can also be involved as was the case in this patient. In addition to the above complications this case highlights the limits of severity scoring systems. The patient’s BISAP score on admission correlated with a mortality risk of < 1%. This underscores the often-volatile clinical course of acute pancreatitis as well as the importance of clinical judgement in assessing a patient's acuity.
Conclusions: Acute pancreatitis, while having an overall low mortality, does pose a challenge to hospitalists given its potential to transform into a severe disease with a myriad of local and systemic complications.