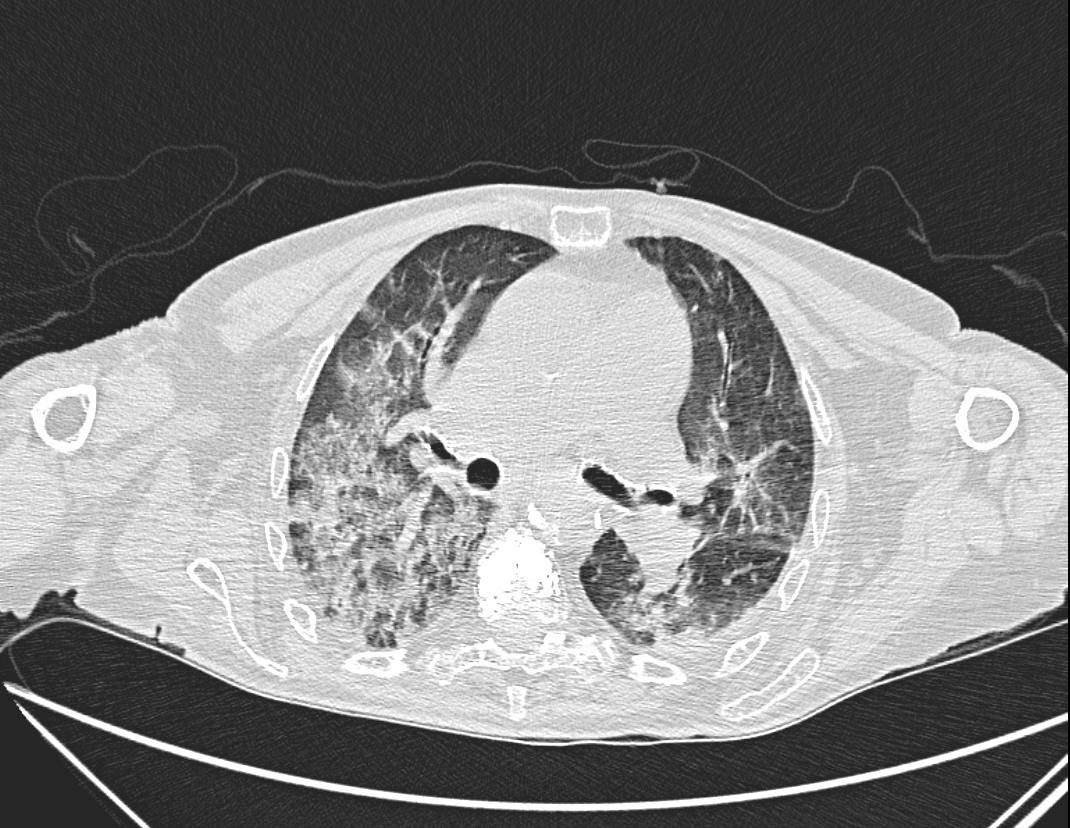
Case Presentation: An 88-year-old female with autoimmune iritis on chronic methotrexate presented after a ground level mechanical fall. Vitals were unremarkable except for O2 saturation of 80% on room air, which improved with 3 lpm of O2. Initial pulmonary exam was unremarkable; her right wrist was swollen and tender. Initial work up showed an elevated D-Dimer of 30,793 ng/mL. Testing for COVID-19, respiratory PCR, procalcitonin and proBNP were unremarkable. Chest x-ray showed bilateral diffuse interstitial prominence and pulmonary congestion. Ventilation-perfusion scan ruled out thrombosis. Right wrist x-ray showed a radius fracture. Echocardiogram showed pulmonary hypertension. She was admitted for respiratory failure and started on diuresis for pulmonary edema. Her wrist fracture was treated conservatively. Three days later, her respiratory status worsened, requiring 15 lpm HFNC. Chest CT showed mid-lower lung bronchiectasis on a background of ground glass, reticular, and consolidative opacities. Pulmonology was consulted; methotrexate and diuretics were held. Further work up included pneumonia management and autoimmune testing. HLA-B27 was positive, while ANA, ANCA with MPO and PR3, RF, Anti-CCP, SCL-70, and hypersensitivity pneumonitis panel were negative. The presumptive diagnosis was acute respiratory failure due to progressive non-specific interstitial pneumonitis (NSIP) with pulmonary hypertension due to methotrexate toxicity. Methylprednisolone 60 mg was started with significant clinical and radiographic improvement. She was discharged with 1-2 lpm O2 and a steroid taper.
Discussion: A well described adverse effect of methotrexate is drug-induced lung injury (DILI). Symptoms are unpredictable and variable, not correlating with dose or duration, which may lead to delayed recognition and treatment of the DILI. The pathophysiology of the lung injury is unclear. Research suggests methotrexate pneumonitis is a type of hypersensitivity disease given the eosinophilia and lymphocytosis in BAL fluid. CT Chest commonly shows parenchymal and reticular opacities in a variety of patterns, including NSIP. NSIP typically features peripheral and symmetric ground glass opacities in an apicobasal gradient. Findings of bronchiectasis and linear reticulations may suggest fibrotic NSIP. Pulmonary hypertension can be a feature of advanced NSIP and may account for pulmonary congestion. Autoimmune pneumonitis was less likely given her advanced age and lack of other characteristic symptoms/serologies. HLA-B27 antigen positivity is typically associated with fibrobullous lung disease in the context of spondyloarthropathies, which was not seen in our patient. Primary treatment for DILI is discontinuation of the offending drug. Improvement can occur over several weeks. Systemic glucocorticoids are reserved for patients with severe symptoms, requiring oxygen supplementation, or who are worsening clinically after methotrexate is discontinued, as in our case.
Conclusions: Diagnosing drug-induced lung disease can be challenging, as the clinical presentation and radiologic findings are typically nonspecific. We present this case to review a rare but well described phenomenon and emphasize the need for comprehensive history and review of radiologic and histologic findings to help rule out other causes, so that prompt treatment can be initiated.