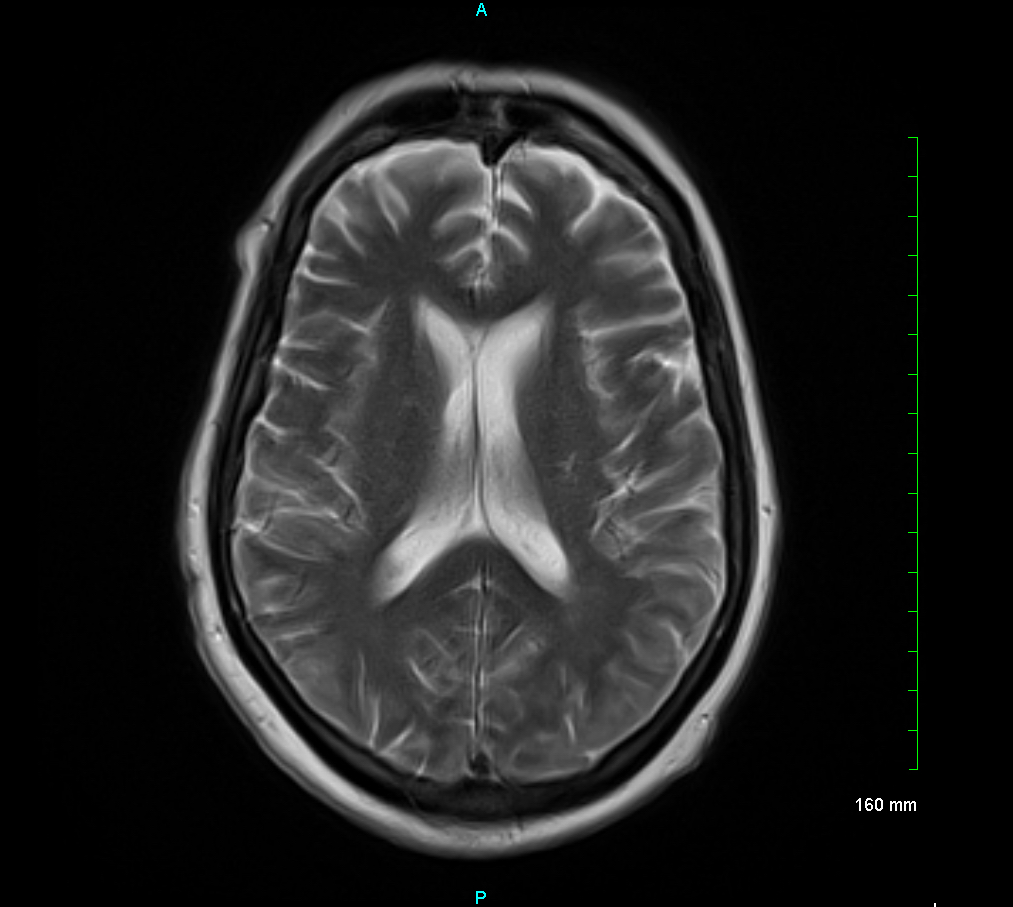
Case Presentation: A 56-year-old female with stage IIB T2N0M0, grade 3, and triple negative breast cancer, was treated with lumpectomy and neoadjuvant chemoimmunotherapy (dose-dense doxorubicin and cyclophosphamide followed by carboplatin/paclitaxel/pembrolizumab). This resulted in near-complete remission. However, evidence of residual disease was found and she was started on pembrolizumab and capecitabine for 3 months. She presented to the emergency department with altered mental status. Metabolic, infectious, and structural work-up including brain MRI was unremarkable (figure 1). Lumbar puncture showed mildly elevated protein levels. Paraneoplastic serum antibody tests were all negative. Electroencephalogram was consistent with diffuse cerebral dysfunction with few epileptiform discharges. The patient was intubated for airway protection. Neurology and oncology were consulted and recommended discontinuation of pembrolizumab and initiated treatment with 1g intravenous methylprednisolone daily for 3 days and intravenous immunoglobulins (IVIG) for 5 days to treat for autoimmune encephalitis secondary to pembrolizumab. The patient’s symptoms did not improve during this time. Further treatment was taken with a 5-day plasma exchange course, and her mental status gradually improved. She was extubated and discharged to acute rehab on a regimen of 60mg prednisone daily that was subsequently weaned by 10mg each week with full cognitive and motor recovery.
Discussion: Pembrolizumab is a monoclonal antibody that targets programmed cell death 1 (PD-1) receptor and is used to treat malignancies such as breast cancer [1]. Cases of pembrolizumab-induced encephalopathy are rare with an estimated prevalence of 0.05% [2]. Two landmark studies in triple-negative breast cancer and the use of pembrolizumab include the I-SPY2 and KEYNOTE-355 trials. Reported immune-mediated adverse events included thyroid disease, pneumonitis, colitis, and severe skin reactions; there were no reports of encephalopathy [3,4]. An extensive literature review was performed, and this is the first case of pembrolizumab induced encephalopathy in the treatment of triple-negative breast cancer. Prompt treatment is required for improved outcomes however this can be difficult as the diagnosis is challenging. Neurological immune-related adverse events (NAEs) typically appear 6-9 weeks after the initiation of immunotherapy [5]. Mainstay therapy for immune checkpoint inhibitor (ICI) related neurotoxicity includes discontinuation of immunotherapy and administration of high-dose corticosteroids [6]. In refractory cases, consider intravenous immunoglobulin, plasma-exchange therapy, or other immunosuppressant drugs. In this case presentation, steroids and IVIG treatment alone did not appreciably show improvement in patient’s symptoms within 5 days of therapy. However, rapid improvement was noted after initiation of plasmapheresis. Furthermore, we permanently discontinued her pembrolizumab as recommended after any grade 3 to 4 (severe or life-threatening) immune related adverse effect (irAE) [7].
Conclusions: This case report focused on pembrolizumab-induced encephalopathy during the treatment of breast cancer that required steroids, IVIG, and subsequently plasmapheresis for improvement of patient symptom’s. This case highlights the importance of monitoring for neurological immune-related adverse events (NAEs) when patients progress throughout treatment.