Case Presentation:
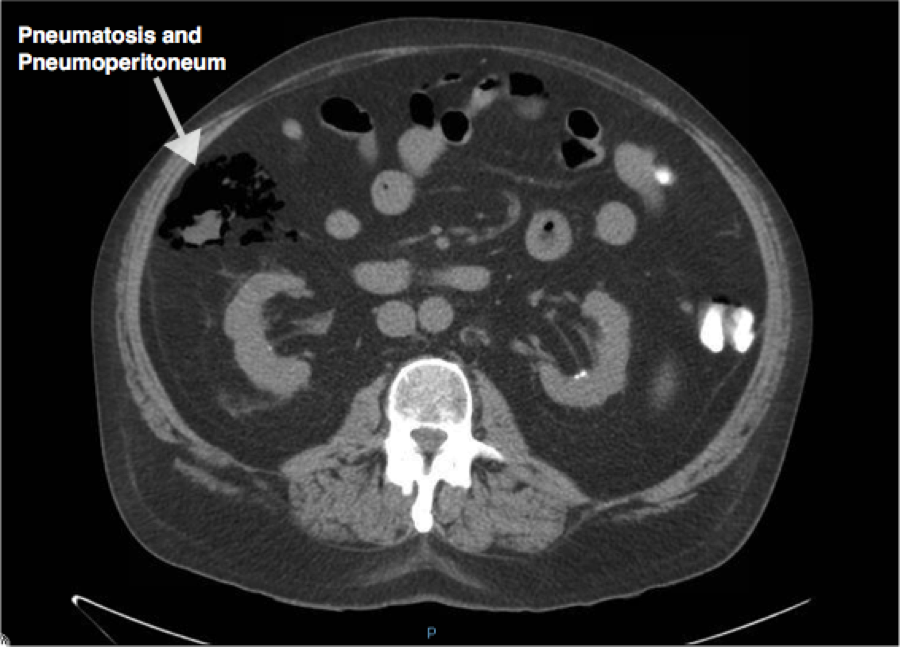
A 56 year old caucasian male with extensive sarcoidosis of the lungs, heart, pancreas and liver had a surveillance 6 month CT scan of the chest+abdomen+pelvis to look for disease progression. Incidentally, he was found to have pneumatosis of the hepatic flexure of colon with surrounding pneumoperitoneum in the absence of associated inflammatory changes or abscesses. He was completely asymptomatic on presentation. His medical history was significant for complete heart block with defibrillator secondary to cardiac sarcoidosis and otherwise negative for peptic ulcer disease, trauma, inflammatory bowel disease, malignancy, radiation, recent GI procedures or surgeries. During his previous colonoscopy (5 years ago) he was found to have a 2 mm polyp that was successfully removed with no signs of diverticulosis or inflammation. Review of systems was otherwise negative and physical examination was completely benign.
He has been on Prednisone 40 mg taper for the past 8 months (currently taking 35 mgs) and was recently started on Methotrexate 7.5 mg weekly 6 weeks prior in an attempt to wean him off the steroids. Laboratory tests showed a white cell count of 10.3 with normal differential and no left shift. Extensive workup including a surgical consult, a GI series with KUB and repeat CT scan abdomen+pelvis did not show any new findings. The only explanation for his presentation was the recent use of Methotrexate that caused intestinal perforation as reported in rare cases before. The medication was discontinued and the patient was scheduled for primary care follow up with repeat CT scan in a week and colonoscopy.
Discussion:
Methotrexate (MTX) can cause dose-dependent hepatotoxicity and gastrointestinal side effects such as nausea, vomiting, diarrhea, stomatitis, glossitis and mucositis. Here we present a rare case of pneumatosis cystoides intestinalis (gas containing cysts in the intestinal wall) and pneumoperitoneum in a patient being treated with MTX for extensive sarcoidosis. Interestingly, in less than 10% of cases, pneumoperitoneum and pneumatosis can be non surgical in etiology and manifest as a benign abdomen with normal white cell count. The concurrent use of high dose prednisone could also potentially mask the natural inflammatory response as was seen in our patient. Gastrointestinal sarcoidosis was also considered in the differential, but given his recent colonoscopy and ongoing use of high dose steroids, it was unlikely to be the case.
MTX acts by causing a sprue-like intestinal syndrome with an atrophied thin wall, reactive atypia and mild pleomorphism. Experimental models involving rats have shown that concurrent use of retinoids helps prevent MTX induced reduction in crypt cell purines and pyrimidines thereby preventing perforation. In humans there is no strong evidence, but the use of growth factor extract, prostaglandins, proanthocyanidin, TGF-alpha and zinc to prevent MTX induced gut toxicity have been explored.
Conclusions: Pneumatosis and pneumoperitoneum can often present as a benign abdomen secondary to medication side effect, such as from methotrexate. When suspected, reducing or stopping the medication may help prevent gut damage and toxicity.