Background: The Accreditation Council for Graduate Medical Education (ACGME) requires residency programs to collect work hour data from trainees, with strict policies that no trainee should exceed an 80-hour work week (on average). Evaluating efforts to reduce work hours frequently relies on self-reported hours from trainees, which is subject to recall bias, inconsistency, and variable reporting. This retrospective approach limits programs’ ability to support trainees who are approaching violations and makes it difficult to rapidly assess the impact of interventions aimed at work hour reduction. Following repeated citations by the ACGME for 80-hour violations, we restructured our inpatient medicine teaching service to better comply with work hours limits. We identified a need for novel approaches to assess the impact of our restructure on trainee work hours and to both identify drivers of work-hour violations and intervene to proactively prevent violations.
Purpose: To utilize novel proactive and reliable methods to measure internal medicine trainee work hours, identify drivers of work hour violations, and intervene to prevent violations.
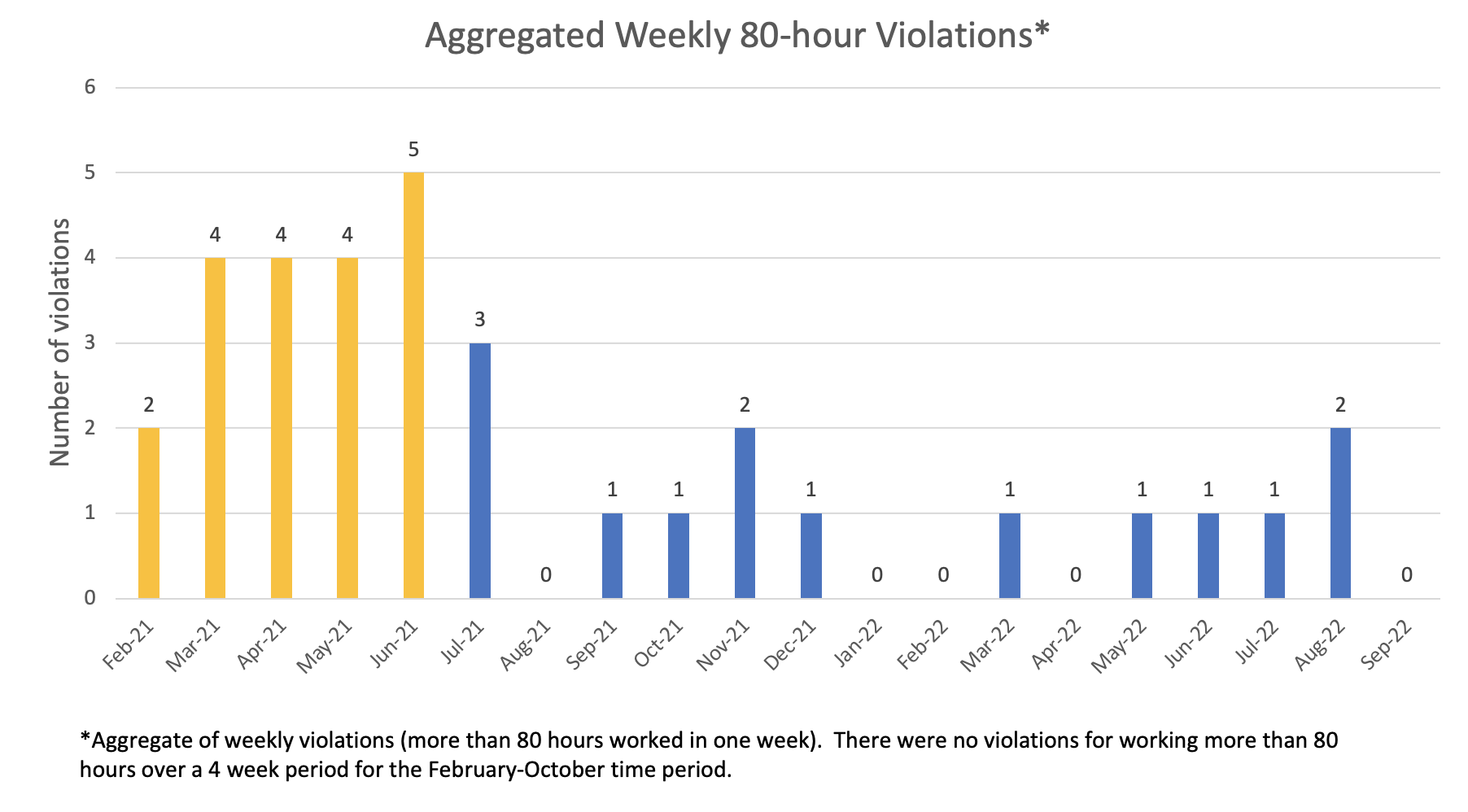
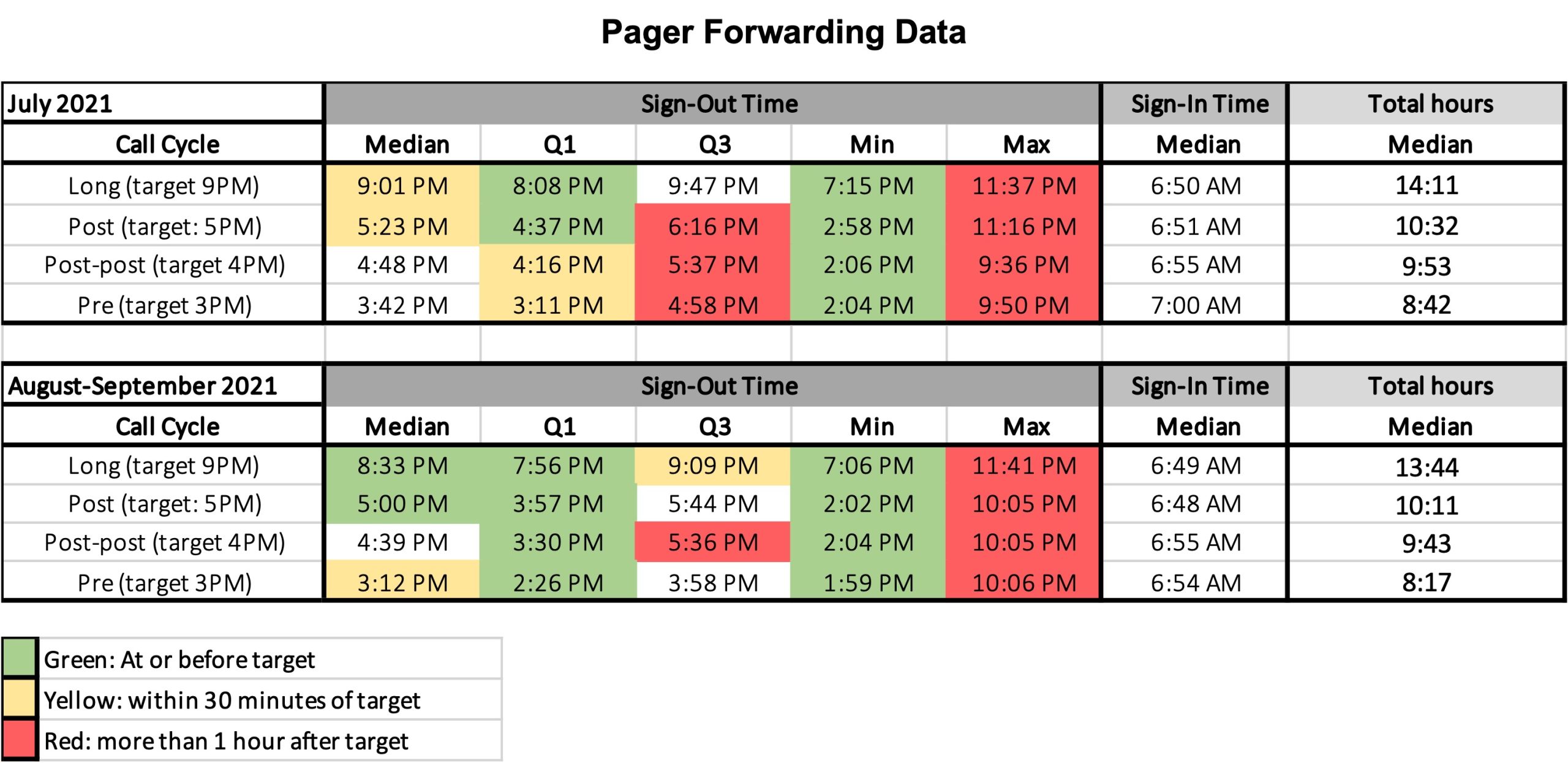
Description: We implemented a restructure to the inpatient medicine teaching service on July 1, 2021. Major changes to the 8-team teaching service structure included: transition to a day/night system from 28-hour call, reduction in admitting hours on long call day (5pm instead of 8pm end), set sign-out times based on day in call cycle, change to a 28-day rotation (from 1-month), and addition of a fifth day off per rotation for each trainee. Team structure remained unchanged, consisting of 1 attending (92% are hospitalists), 1 resident (PGY2-3), and 2 interns. After implementation of the new wards structure, work hour violations by intern and resident trainees on the teaching service fell dramatically: from July 2021-September 2022, there was an average of 0.93 weekly violations compared to 3.8 for the 5 months prior to the restructure (p< 0.001) (Figure 1). Pager forwarding data showed median pager forwarding times were within 1 hour of target times during the period of July-September 2021 (Figure 2).We monitored for work hour violations via a multimodal approach including (1) a real-time dashboard based on user log-in to the electronic medical record (EMR), (2) pager forwarding data, and (3) retrospective self-reported hours (via MedHub). The dashboard was a novel tool that allowed for nearly real-time intervention as needed, such as providing additional coaching or clinical support, reducing new patient volume, or requiring early dismissal or an additional day off. This allowed for proactive intervention for trainees approaching 80-hours to avoid violations. Pager forwarding data measured adherence to standardized sign-out times. Combining these two measurement methods allowed for better understanding of drivers of work-hour violations such as identifying high documentation burden and certain days in the call cycle (e.g. solo resident on interns’ day off) as particular drivers of work hours. This allowed subsequent targeted interventions of these drivers.
Conclusions: A thoughtfully structured inpatient medicine teaching service can support trainee adherence with work hour limitations. Novel tools to measure work hours, such as a real-time dashboard reporting EMR-login hours and pager forwarding data, can allow for new ways to measure work hours, understand drivers of work-hour violations, and enable just-in-time intervention to prevent work-hour violations.