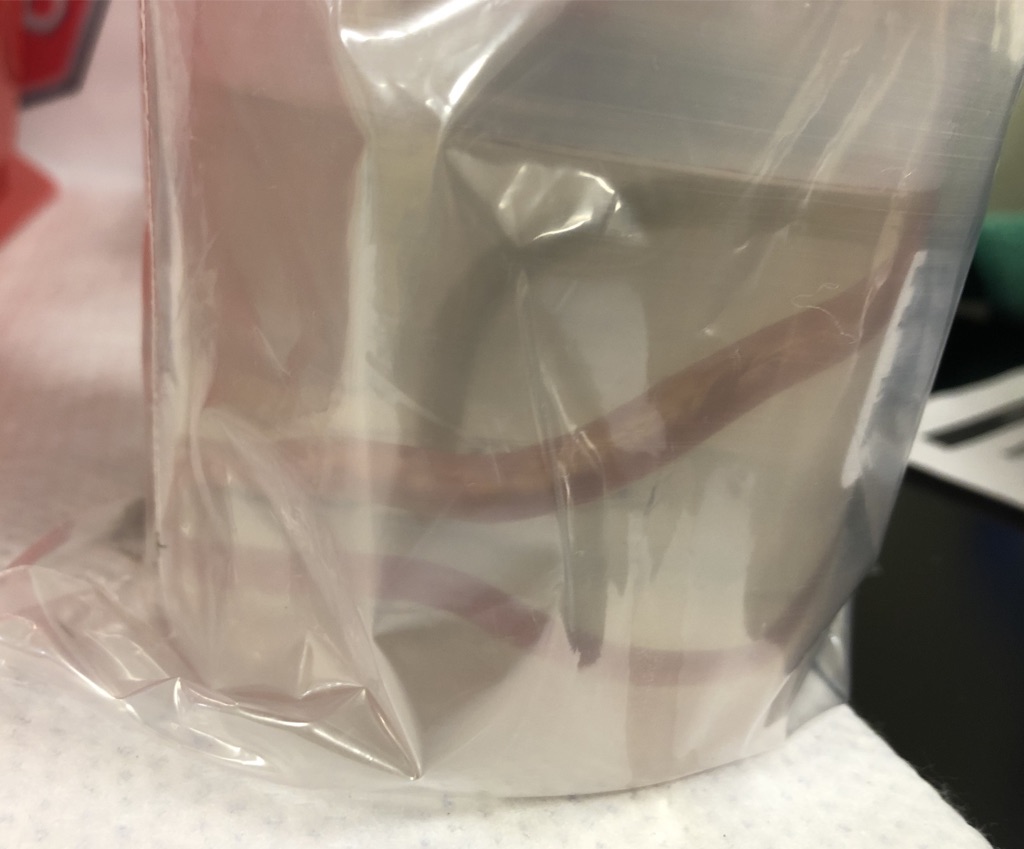
Case Presentation: A 60-year-old African woman presented to the emergency department with three days of abdominal pain, nausea, and vomiting. She had recently returned from a ten-month trip through rural Ethiopia where she consumed unpasteurized milk and well water with exposure to goats, cats, and livestock. Her medical history was otherwise unremarkable. On exam, she was tachycardic (110 bpm), hypotensive (53/34 mm Hg), and afebrile. Her exam was also notable for midline abdominal tenderness. Laboratory findings were notable for white blood cell count of 22 x 10^9/L without eosinophils, hemoglobin of 13.3 g/dL, platelet count of 35 x 10^9/L, total bilirubin of 1.4 mg/dL, direct bilirubin of 0.6 mg/dL, alkaline phosphatase of 143 U/L, aspartate aminotransferase of 38 U/L, alanine aminotransferase of 40 U/L, and lactate of 8.3 mmol/L. Blood cultures on admission grew Klebsiella pneumoniae. Non-contrast CT of the abdomen was notable for hepatomegaly with cavitary lesions in the left lobe of the liver consistent with abscesses, pneumobilia with biliary ductal dilation, and a hydropic gallbladder. Percutaneous drainage of the gallbladder and left liver abscess was performed with frank pus aspirated from the abscess. MRCP revealed tubular filling defects in the dilated extrahepatic biliary ducts. ERCP revealed a choledochoduodenal fistula with a foreign body versus parasite visible in the common bile duct. Balloon sweep of the bile duct yielded sludge followed by passage of a 13-inch roundworm. The worm was retrieved and sent to the microbiology lab, where it was identified as Ascaris lumbricoides. The patient improved markedly and rapidly after biliary decompression and was then treated with two doses of oral albendazole. She passed additional Ascaris lumbricoides in her stool during the hospitalization. She was discharged on oral Augmentin with plans for drain removal six weeks later. At the two-week follow-up, she was symptom-free and clinically improved.
Discussion: Ascariasis is a common parasitic infection in developing countries, but relatively uncommon in the United States. In the preceding clinical vignette, we describe a case of hepatic abscess that developed secondary to obstruction from hepatobiliary ascariasis. Ascaris lumbricoides infection is estimated to affect up to 800 million people globally, primarily in Asia. Transmission occurs via contaminated water or soil with up to a 24-month incubation period in the intestines. Although eosinophilia is classically associated with parasitic infections, the absence of eosinophilia does not rule out Ascaris infection. Hepatic abscesses and bacteremia as a result of Ascaris infection have only been described in one other case report in the literature.
Conclusions: Though a rare etiology for hepatic abscess formation, hepatobiliary ascariasis should be considered in individuals who have spent time in endemic regions and have risk factors for this parasitic infection.