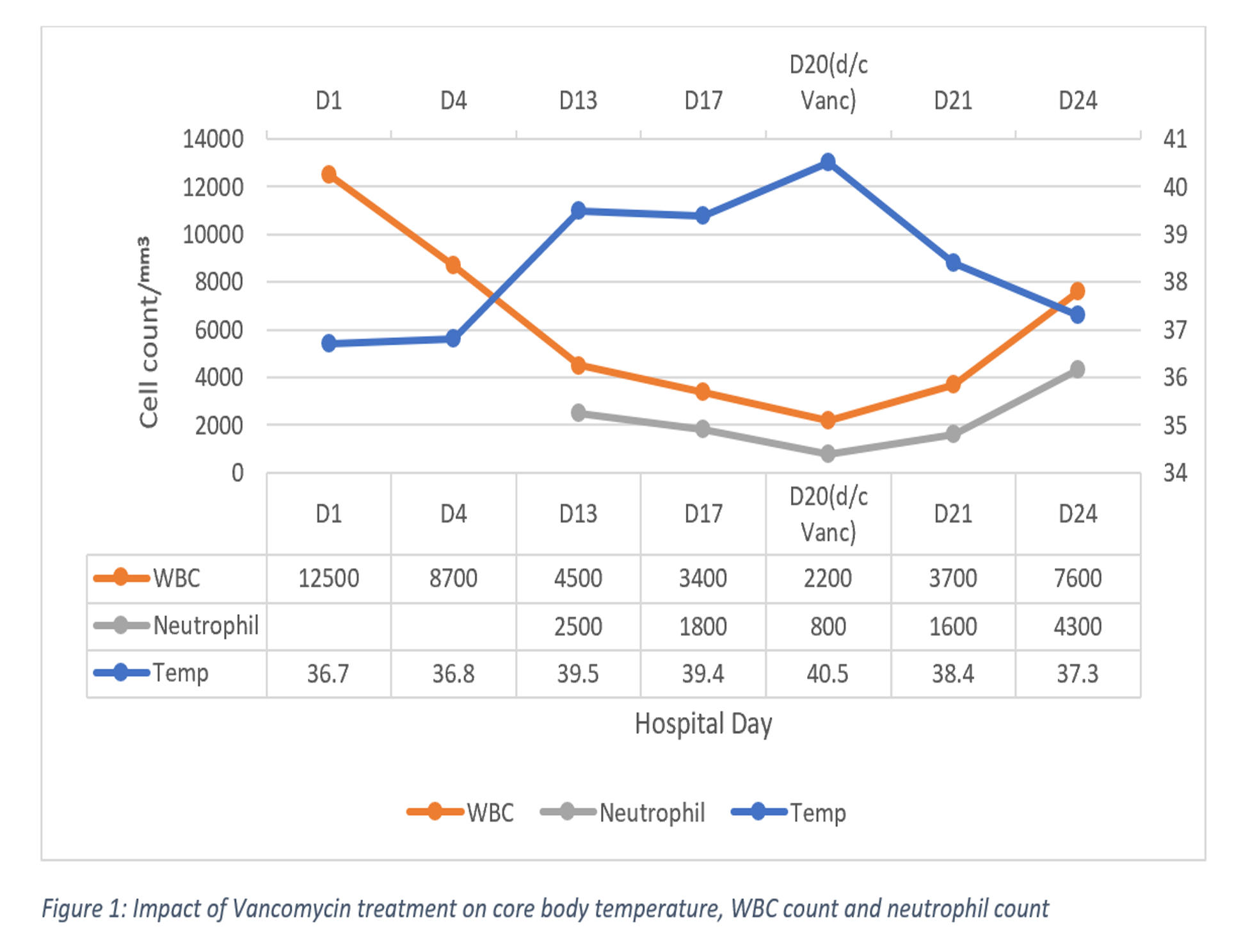
Case Presentation: A 24-year-old man presented with MRSA osteomyelitis of his right tibia two months after suffering an open fracture during a helicopter crash into a mountain. He was started on intravenous vancomycin. The patient did well for thirteen days however then started to have recurrent fever spikes up to 104.9 °F with concurrent sinus tachycardia. Exam was benign except for significantly enlarged, bilateral tender anterior cervical lymph nodes. WBC count was 4,500 with a neutrophil count of 2,500. Inadequate infection control, pulmonary embolism, endocarditis, pneumonia and drug fever among others were included on the differential. Vancomycin trough was within therapeutic range. Repeated blood cultures were negative, CT chest was normal, and UA was unremarkable. HIV panel, syphilis serology, herpes panel, EBV antibody, histoplasmosis/Q fever/tularensis/bartonella serologies were negative. Because no apparent cause of the fever and neutropenia was identified, patient was symptomatically managed and continued to receive vancomycin. In subsequent days, WBC and neutrophil counts continued to decline. On hospital day 20, WBC was 2,200 with a neutrophil count of 800. Given that his fever began during the hospital stay and that no other obvious causes were identified, vancomycin-induced fever and neutropenia were considered. Vancomycin was discontinued and patient was instead started on daptomycin. The patient’s fever subsided, and he clinically improved significantly over the next 24 hours. WBC improved to 7,600 with neutrophil count of 4,300 four days after stopping vancomycin. Interestingly, his cervical lymphadenopathy also improved although we still could not identify the cause; we suspected an unidentified viral cause. Patient was discharged to a rehabilitation facility and was doing well on follow-up.
Discussion: Vancomycin is widely used for the treatment of resistant gram-positive infections including MRSA. Although uncommon, there are reported cases of fever and neutropenia secondary to prolonged vancomycin use. Previous literature review suggests vancomycin-induced neutropenia occurs mostly beyond 20 days of therapy but can happen as soon as 7 days after initiating the treatment. Drug-induced fever is most commonly seen after 7 to 10 days of therapy. Our case is unique in that vancomycin-induced fever coincides with severe neutropenia, and that both uncommon adverse effects quickly resolved after substitution of vancomycin with daptomycin.
Conclusions: Vancomycin-induced fever and neutropenia are uncommon, possibly immune-mediated, potentially serious adverse effects most likely seen with prolonged exposure. Patients receiving vancomycin for longer than 7 days should be closely monitored for fever and neutropenia with at least weekly CBC with differential. The drug should be discontinued if vancomycin-induced fever and neutropenia are suspected.