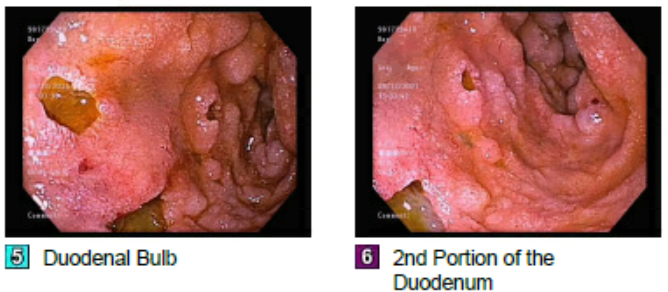
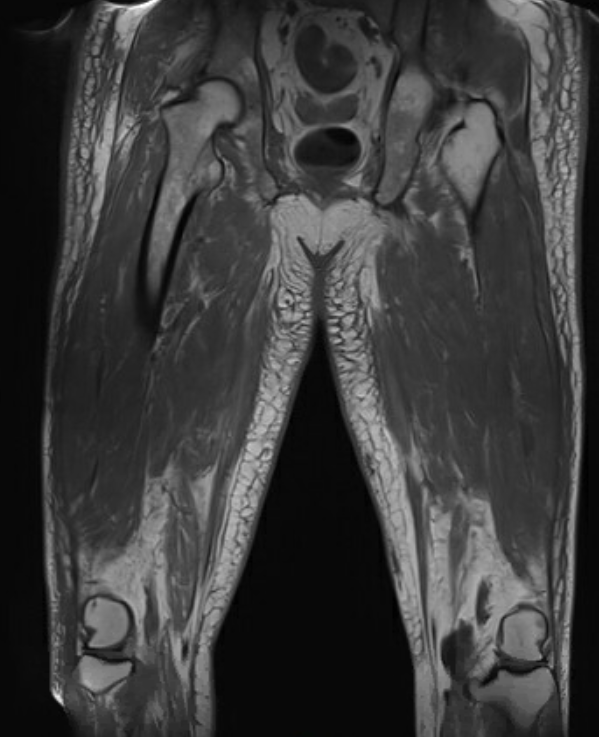
Case Presentation: A 63 year old male with no past medical history was admitted with five months of bilateral upper and lower extremity weakness as well as a pruritic, erythematous rash on his face, arms, and back. This was followed by progressive dysphagia. Initial workup, including a pectoralis muscle biopsy showing necrotizing myopathy, and MRI femur with diffuse muscle edema, revealed idiopathic dermatomyositis. He was treated with intravenous immunoglobulin (IVIG) and high-dose steroids. He required PEG tube placement due to severe dysphagia, and was discharged to inpatient rehab on a prolonged steroid taper.Two months later, he re-presented for vomiting and aspiration pneumonia due to progressive dysphagia. CT abdomen showed duodenitis and diffuse descending and sigmoid colitis. Gastroenterology suspected GI involvement of dermatomyositis. He underwent upper endoscopy which revealed severe diffuse gastritis with numerous non-bleeding esophageal, gastric, and duodenal ulcers. Biopsies showed intestinal metaplasia and no evidence of H. pylori. His hospital course was complicated by malabsorption and inability to tolerate enteral nutrition, as well as recurrent aspiration pneumonia causing respiratory failure. A central line was placed in preparation for TPN, but he developed gram-negative bacteremia likely from an intestinal source, which precluded TPN initiation. He developed melena and underwent two additional upper endoscopies which showed progressive gastritis and duodenitis with active bleeding, and many new cratered esophageal, gastric, and duodenal ulcers concerning for CMV infection; however, viral stains were negative.He was initially maintained on high-dose steroids for dermatomyositis which were tapered due to infection and GI ulcers. He completed another course of IVIG, and initiation of rituximab was considered. However, due to critical illness, myopathy, and severe ulcers, he was not started on other immunosuppression. His malnutrition contributed to his progressive debility and poor overall outcome. He eventually elected to transition to comfort care and was discharged to hospice where he ultimately passed.
Discussion: Dermatomyositis (DM) is a rare inflammatory myopathy that typically presents with muscle weakness and skin rash. Morbidity and mortality in DM increases with involvement of other organs such as the heart, lungs, and GI tract. Dysphagia can be a presenting symptom of DM and is thought to be due to loss of muscle tone, with estimated incidence ranging from 19-62%; however, it rarely progresses to the point of causing malnutrition and aspiration. [1-3] GI ulceration has been reported in pediatric patients with DM. The rare cases noted in adults have been associated with poor outcomes. [4-5] Glucocorticoids are the mainstay of treatment for DM. [6] Biologics may be considered for those with refractory disease or who are unable to tolerate steroids. The risks and benefits of treatment with these agents should be carefully considered, particularly in critically ill patients.
Conclusions: Internists should recognize the potential for GI involvement of dermatomyositis and the subsequent difficulty with managing nutrition and malabsorption. Upper and lower endoscopy may be useful to evaluate for mucosal involvement early in the disease course. For patients with severe dysphagia leading to malnutrition, providers may consider early initiation of TPN while taking into account the risk of infection with immunosuppression.