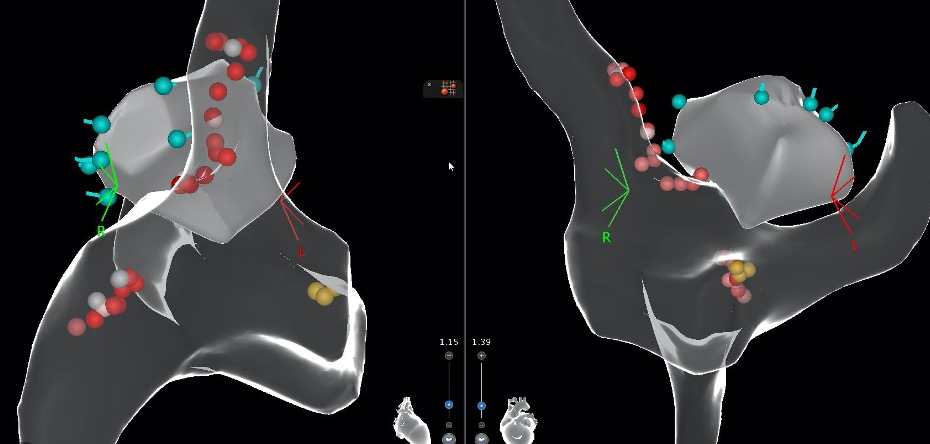
Case Presentation: A 62-year-old man with hypertension, type 2 diabetes mellitus, benign prostatic hyperplasia (BPH), and history of cerebellar stroke syndrome secondary to a remote vertebral artery dissection presented for positional lightheadedness. Four months prior to presentation, he developed positional lightheadedness associated with standing that forced him to widen his gait for steadiness; these episodes lasted for several minutes before self-resolving. He also noted extreme lightheadedness upon turning his head while supine to either side; these episodes lasted for approximately 60 minutes before resolving. He reported adequate fluid intake; he denied emesis, cough, alcohol, illicit drug use or other triggers prior to these episodes. He was not taking any beta-blockers or calcium channel blockers; he was taking tamsulosin for BPH, which was discontinued without resolution of his symptoms. He underwent autonomic testing which revealed an abnormal baroreceptor reflex response to Valsalva maneuver, including an exaggerated fall in blood pressure (BP) and the lack of hypertensive overshoot post-Valsalva. Parasympathetic modulation of heart rate with slow deep breathing showed exaggerated parasympathetic response. Right but not left carotid sinus massage reproducibly resulted in a 2-3 second pause in heart rate associated with a 15-30 mmHg fall in systolic BP. These findings were consistent with right carotid hypersensitivity and adverse parasympathetic autonomic influence. He underwent minimally-invasive cardioneuroablation (CNA) in the electrophysiology lab. He noted immediate improvement, reporting minimal episodes of dizziness and no syncope, which persisted up to his most recent follow-up four months post-procedure. An implanted loop recorder (ILR) has monitored the effectiveness during the post-treatment period, showing no evidence of sinus pauses or ventricular block for 5 months.
Discussion: Although carotid sinus hypersensitivity (CSH) is far less common than neurally-mediated (“vasovagal”) reflex syncope, it can be associated with significant impairment in the quality of life (QoL) of affected patients. The treatment of cardioinihibitory CSH, the most common type of CSH, usually includes pacemaker insertion for those most severely affected. A new and less invasive treatment, CNA, has been used extensively in selected patients with vasovagal syncope but has not been frequently employed in patients with cardioinhibitory CSH. In fact, successful use of CNA in the patient reported here is, to our knowledge, only the third case reported in the literature. However, we report the use of continuous ECG monitoring with ILR for 5 months, suggesting treatment durability performed with right atrial approach only.
Conclusions: Reflex-mediated (vasovagal, situational, and carotid sinus hypersensitivity) syncope is common with a significant impairment in the QoL of affected patients. In this case, we presented a patient with cardioinhibitory CSH treated with a novel and minimally invasive procedure; CNA. CNA remains a promising new intervention for selected patients with cardioinhibitory CSH and its application should be further investigated. Patients who remain symptomatic following CNA can always be considered for pacemaker insertion.