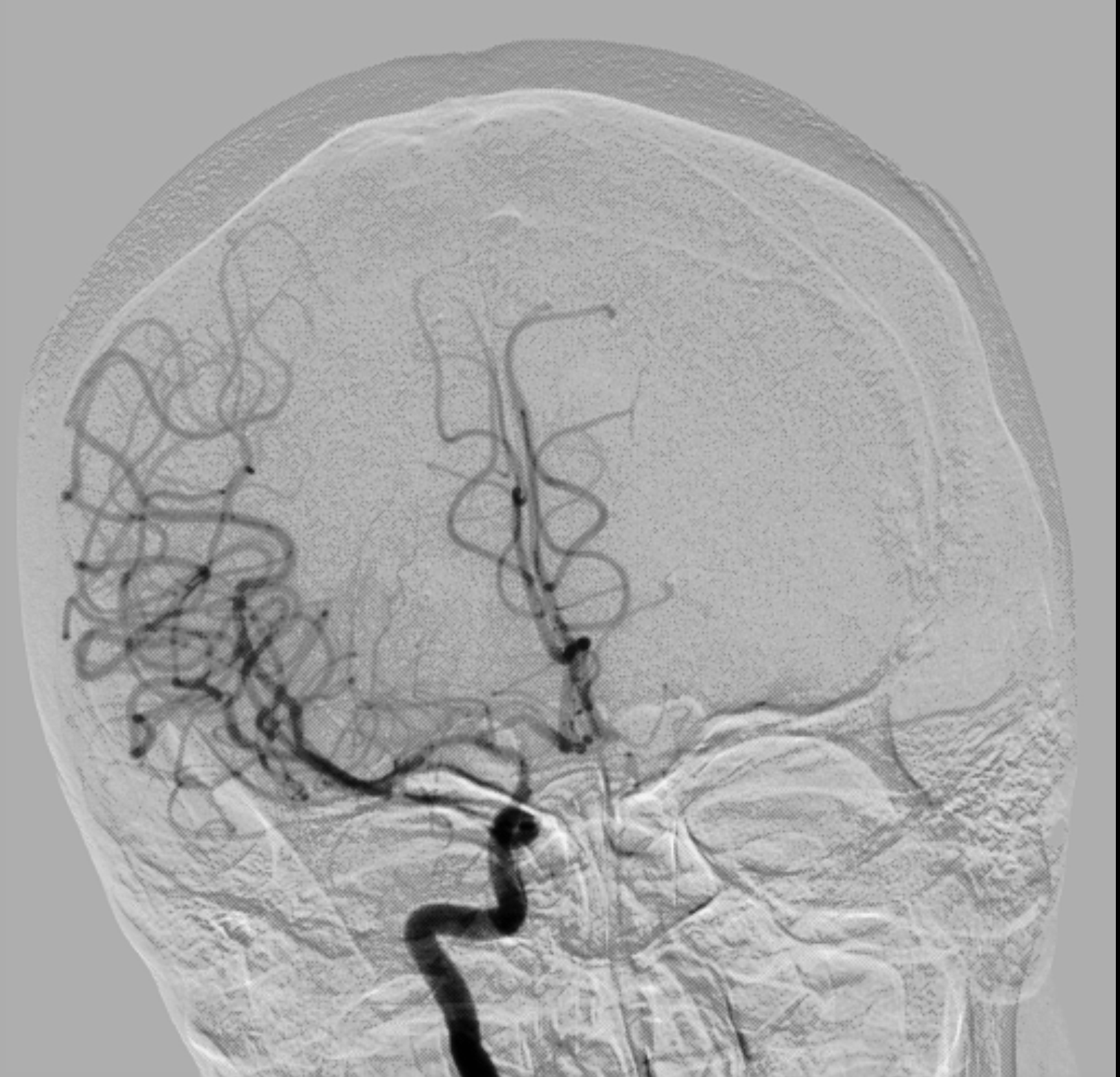
Case Presentation: A 60 -year old Caucasian female presented to the emergency department with right-sided hemiparesis and dysarthria. The patient had been admitted to an outside facility one week prior to presentation for left foot osteomyelitis. That admission was complicated by right upper extremity DVT and she had been started on apixaban. When she presented to our facility, physical examination was remarkable for right upper extremity weakness (4/5), dysarthria and a left-sided breast mass. Significant laboratory data were hemoglobin 10.7g/dl, Platelets 38k/ul, schistocytes 1/hpf, immature platelet fraction 19.6%, reticulocyte count 2.8%, LDH 787U/L and creatinine 0.8mg/dl. MRA showed occlusion of the right internal carotid artery terminus, right M1 segment and left MCA and cerebral angiogram demonstrated Suzuki Stage 4 Moyamoya disease of the bilateral internal carotid arteries.
Discussion: A tentative diagnosis of thrombotic thrombocytopenic purpura (TTP) and Moyamoya disease was made and treatment with plasmapheresis was started. She underwent five pheresis with improvement in the platelet count to 286k/ul by the fifth day. ADAMTS13 activity however returned as normal and FNA of the left breast mass and left axillary lymph node revealed ER-positive breast cancer. Additional laboratory studies were significant for PTT 42s, Beta 2 glycoprotein IGG 32 SGU ( <20) and positive hexagonal phase neutralization which suggested secondary antiphospholipid syndrome (APS). ANA, complement levels and transesophageal echocardiography were normal. Apixaban was replaced with enoxaparin and low dose aspirin commenced. Surgical management was deferred because of patient’s suboptimal clinical status. Three months later, repeat antiphospholipid panel was however negative.
Conclusions: Moyamoya is a rare cerebrovascular condition with occurrence of 0.086 cases per 100,000 persons in the US. It has a bimodal age distribution and in adults occurs most frequently in women. Complications of Moyamoya range from ischemic changes presenting as stroke ,TIA or seizures to the effects of compensatory mechanisms which include hemorrhage and headache.1 APS is a procoagulant condition associated with the formation of antiphospholipid antibodies (APA) and occurring in isolation or secondary to conditions including malignancies. 2,3 In addition to clinical criteria, diagnosing APS requires positive repeat APA after twelve weeks3. Some authors speculate that the development of Moyamoya could serve as a trigger for the development of APA4. The occurrence of thrombosis and Moyamoya in the same patient presents a particular challenge in management because of the heightened risk for thrombotic/ischemic complications and the bleeding risk associated with the use of antiplatelets and anticoagulants4. REFERENCES
1. Pollak L. Moyamoya disease and moyamoya syndrome. N Engl J Med. 2009;361(1):98; author reply 98. doi:10.1056/NEJMra0804622.
2. Reddy P. Laboratory diagnosis of antiphospholipid syndrome. South Med J. 2013;106(7):439-446. doi:10.1097/SMJ.0b013e31829b9c03.
3. Lim W. Antiphospholipid syndrome. Hematology Am Soc Hematol Educ Program. 2013;2013:675-680. doi:10.1182/asheducation-2013.1.675.
4. Wang Z, Fu Z, Wang J, Cui H, Zhang Z, Zhang B. Moyamoya syndrome with antiphospholipid antibodies: a case report and literature review. Lupus. 2014;23(11):1204-1206. doi:10.1177/0961203314540761.