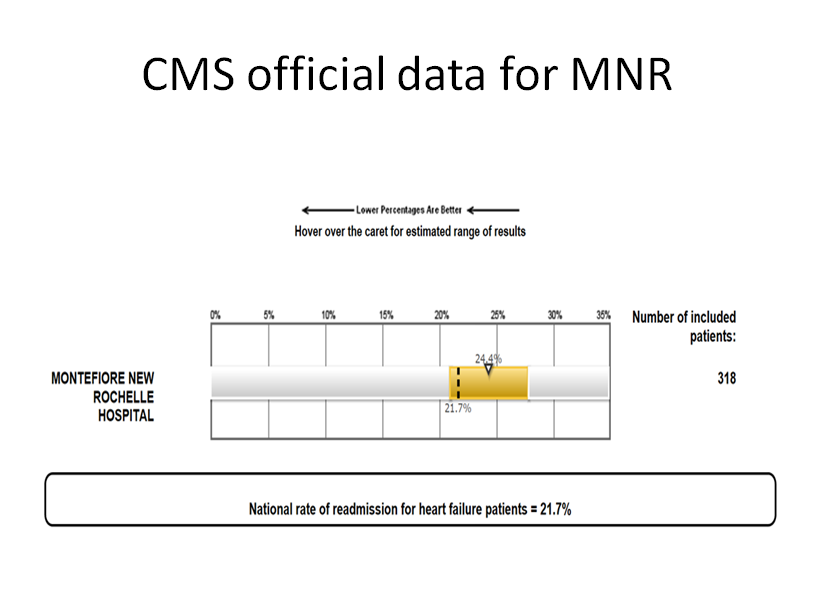
Background: Congestive heart failure (CHF) is a major cause of mortality and morbidity among general population despite recent advancements in goal-directed therapies. The advent of mechanical circulatory devices, the increased availability and improvement in heart transplant techniques have improved some metrics; however, CHF patients continue to have multiple readmissions for acute exacerbations. The frequency of readmission affects the overall quality of life and mortality. The national 30-day readmission rate remains high at 21.4%. Hospitals in the United States are implementing strategies to reduce heart failure readmissions focusing on goal-directed therapy, concerted discharge planning, improved patient communication, physician education, and post-discharge follow up.
Purpose: Our quality improvement project focused on decreasing the 30-day readmission rates for CHF patients admitted to our community hospital by implementing the above measures and studying the utilization of these measures.
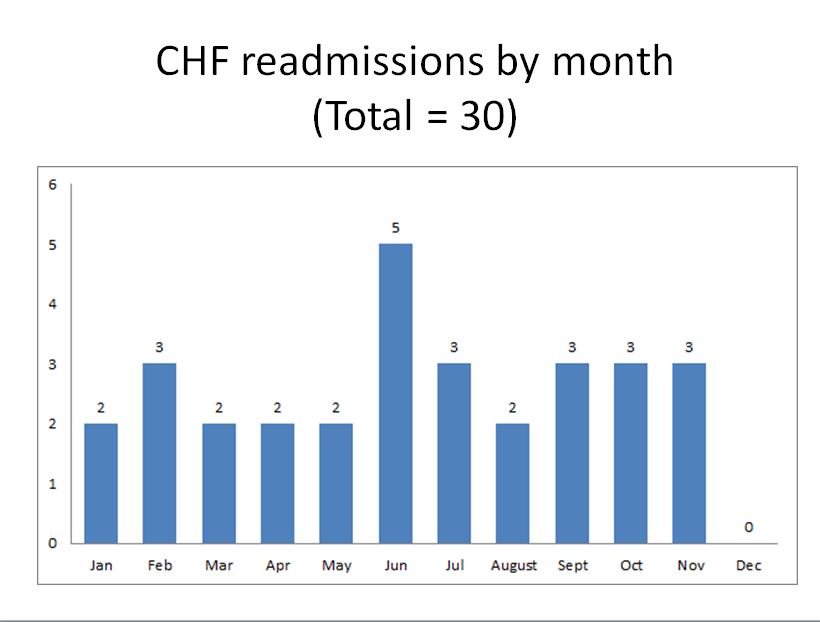
Description: This project was conducted using standard quality improvement tools including Plan-Do-Study-Act cycles (PDSA) and a key-driver diagram. From our previous experience using the Pareto principle, we identified a lack of patient education and post-discharge follow up as the main factors leading to readmission at our hospital. These were identified as areas of improvement. We generated a document in the electronic medical record system, which would flag any admission with the CHF diagnosis. This system also generated multidisciplinary consults focused on patient education (nutrition, pharmacy, and nursing) and social worker referral to coordinate post-discharge care. Patients were specifically educated about diet, heart failure medications and the importance of daily weights by using a “Heart Failure Handbook”. A retrospective study was done with individual root-cause analysis performed for each readmission. CHF readmission was defined as two consecutive hospital admissions within the 30 day period, with an admission diagnosis of CHF.From 1/1/2018 to 12/31/2018, a total of 247 CHF admissions were analyzed. A total of 30 readmission cases that met CHF readmission criteria were identified. Mean readmission length 13 days (SD +-8), the mean age of readmission was 75 (SD +-16), mostly female 77%. Most of the readmissions came from a home with or without home care services. CHF with reduced ejection fraction was present in 57% of cases, while CHF with preserved ejection fraction was present in 40% of cases. Overall CHF readmission mortality is 13.3% while for documented NYHA class III-IV is 18.18%. The palliative team was consulted for 1 out of 30 readmissions. A tendency to change code status upon readmission was observed. With our multidisciplinary approach, there was a significant decrease in all-cause 30-day readmission rate for CHF in our hospital from 21% in 11/2017 to 8-12% in 1/2019.
Conclusions: There was a significant decrease in the all-cause 30-day readmission rate for CHF in our hospital after the implementation of these quality improvement methodologies, multidisciplinary approach, patient education, and post-discharge follow up. Specific patient characteristics were identified in our predominantly elderly population group.