Background: Cardiovascular disease remains the leading cause of death in the United States. Approximately every 40 seconds, an American will have a myocardial infarction. The aim of this project is to assess the progress of the prevention and management of myocardial infarction by using the National Inpatient Sample (NIS) data.
Methods: This is a retrospective study utilizing The National Inpatient Sample (NIS) from 2000 through 2015. Discharges due to myocardial infarction from 2000 to 2015 were identified by using ICD-9 sorted by Clinical Classification Software (CCS). The rate of discharges per 100,000 persons, inpatient mortality, length of stay and hospital cost were trended. Inpatient mortality was classified further by gender and by teaching status of the hospitals (teaching vs non-teaching). The length of stay and hospital costs were also classified. Z-test was used to find the statistical difference in the length of stay between teaching and non-teaching hospitals.
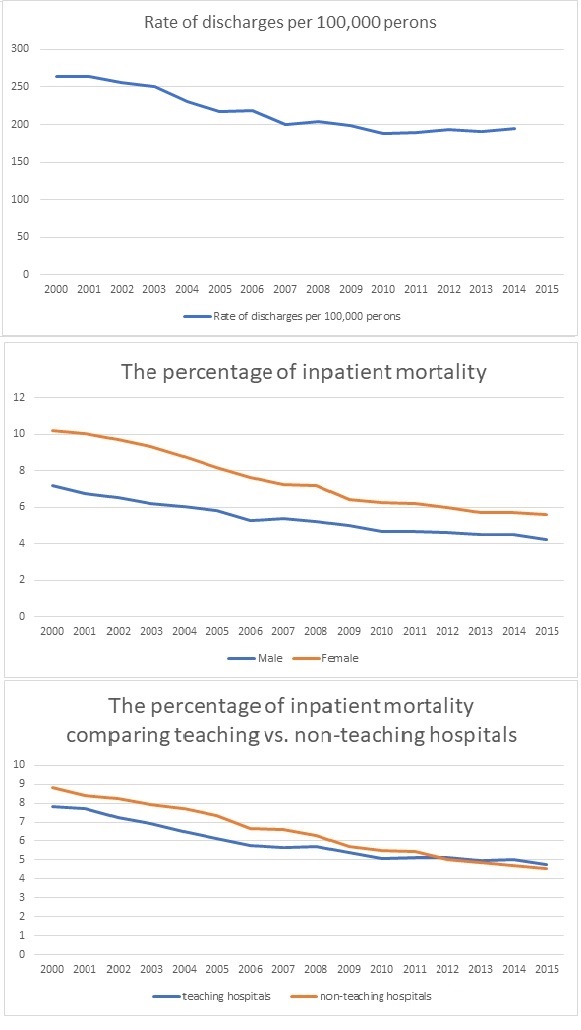
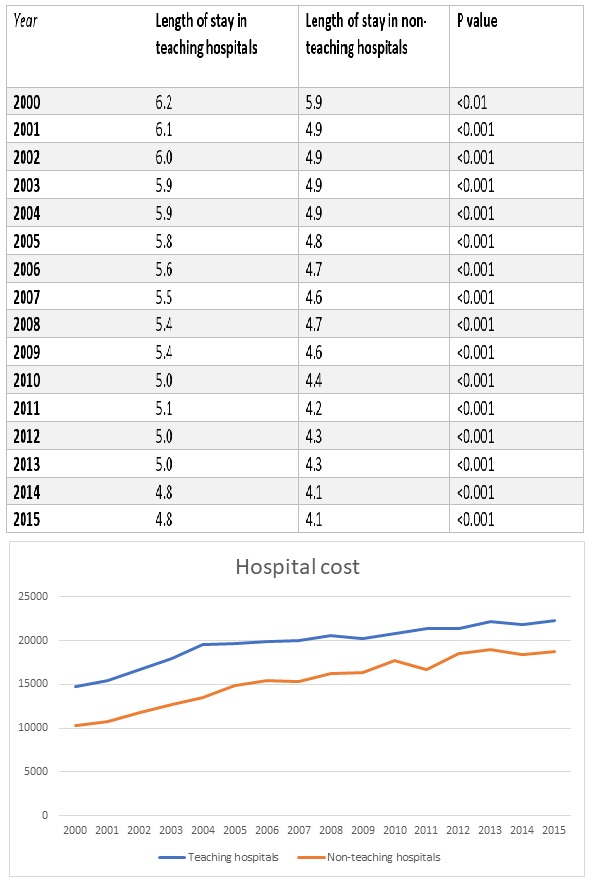
Results: The rate of myocardial infarction discharges per 100,000 persons decreased between 2000 to 2015 (see figure 1). Similarly, inpatient mortality declined in both genders, but the female inpatient mortality rate was significantly higher over the 15 year period (see figure 1). No change was noticed in the mean age for myocardial infarction of either gender over the studied period of time. When comparing teaching and non-teaching hospitals, no significant difference was observed in the inpatient mortality rate. There was a statistically significant difference in the length of stay with correlating differences in the hospital cost (see figure 2).
Conclusions: The decrease in the rate of discharges reflects improvement in the preventative measures and the role of primary and secondary prevention. The decrease in inpatient mortality reflects the advancement in the medical and interventional management of myocardial infarction; however, this improvement in the management has led to a significant increase in hospital costs. The length of stay in teaching hospitals is longer than non-teaching hospitals (see figure 1 and 2), and the difference is statistically significant. There was no significant difference in inpatient mortality. There is no change in the mean age for myocardial infarction for either gender through the studied 15 years. The female gender appears to be a non-modifiable risk factor for inpatient mortality. In general, the results suggest we are heading in the right direction in terms of prevention, medical and interventional management of myocardial infarction at the expense of increasing hospital costs. Additionally, teaching hospitals can do better in terms of length of stay in order to decrease the hospital costs and match the lower costs of non-teaching hospitals.