Background: Sepsis is one of the most common causes for adult emergency department admissions and carries high morbidity and mortality. Appropriate and timely administration of intravenous (IV) antibiotics is one of the cornerstones of initial management of sepsis. Indeed, mortality has been shown to increase by 7-14% for each hour of delay in antibiotic administration. In 2017, Hurricane Maria struck Puerto Rico, producer of >40% of the IV fluid bags used in the US, causing an escalation of a critical shortage of IV fluids nationwide. As a result, hospitals nationwide, including ours, implemented a conversion from IV piggyback to IV push administration of antibiotics in sepsis protocols. As there are no studies evaluating the effect of these changes on sepsis care, we aimed to study the impact of the change from IV piggyback to IV push antibiotic administration in terms of 1) time to first dose of antibiotics and 2) sepsis mortality.
Methods: This was a single-center, retrospective review. Data was extracted from the Mount Sinai Hospital sepsis database of adult patients who screened positive for sepsis and the sepsis bundles applied; cases were included from March-May 2017 (baseline, prior to the change from IV piggyback to IV push) and March-May 2018 (after the change). The timeframes were selected to minimize effects of anticipation (in the baseline period) or nursing staff getting used to IV push. Data collected were 1) time to first dose of antibiotics and 2) sepsis mortality. Additionally, baseline demographics, Charlson-Deyo score, source of infection, clinical data at time of sepsis identification, such as temperature, blood pressure, and lactate were collected. For both study objectives, a quasi-experimental interrupted time series approach with a segmented regression analysis was applied where both time periods were compared in terms of time to antibiotic administration and sepsis mortality. To further test for robustness of results, the same analysis was applied to an antibiotic unaffected by the change in medication administration (a control group). P-values less than 0.05 were considered statistically significant.
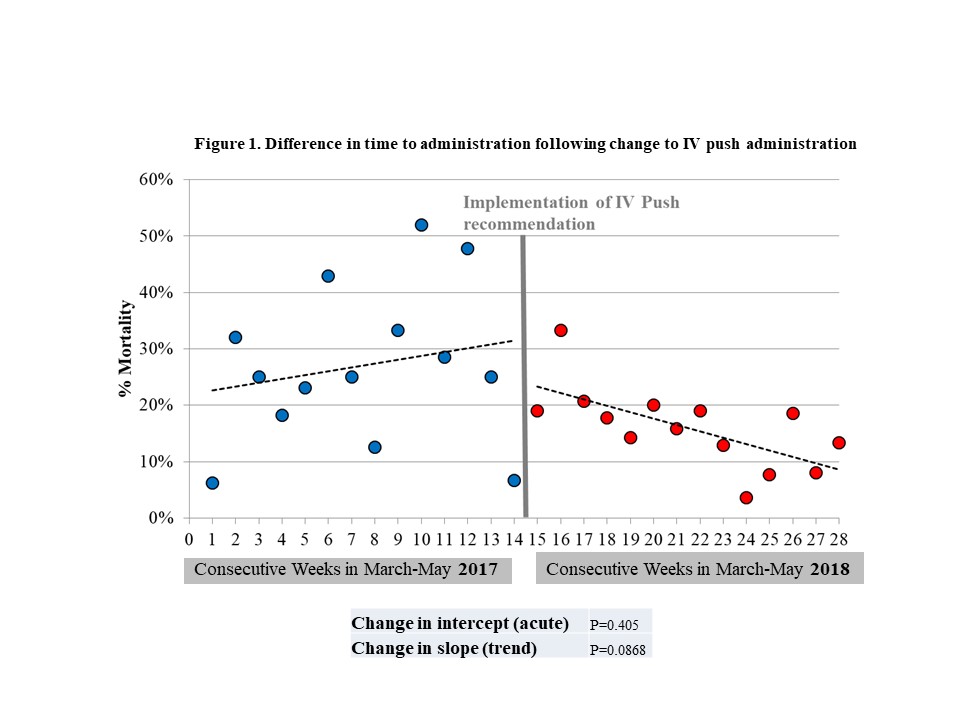
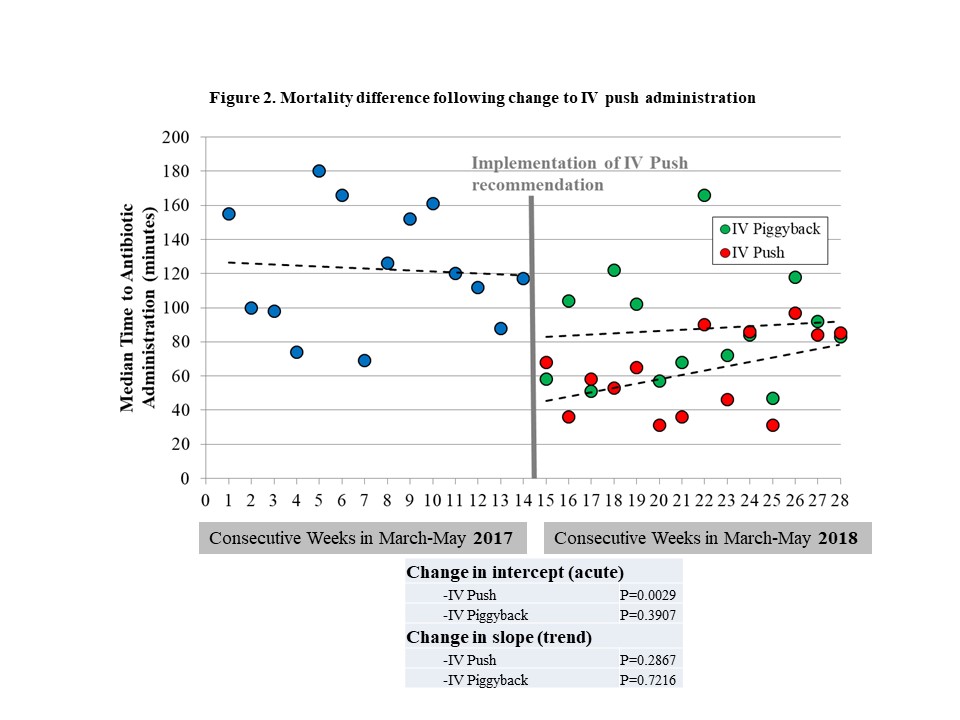
Results: : Overall 259 and 343 patients were included in the baseline and intervention period, respectively. There was a significant acute reduction in time to first dose antibiotic in patients who received IV push compared to baseline (Figure 1; p=0.0029). However, by the end of the three-month intervention period, there was a trend towards convergence to baseline (p=0.287). No statistically significant difference was seen in terms of mortality, however, a trend towards reduced mortality (p=0.087) was observed (Figure 2). The most common antibiotics administered were cefepime, vancomycin, and piperacillin/tazobactam in both study periods. In terms of group differences, the only difference between the baseline and intervention group was seen for systolic and diastolic blood pressure, with the cohort receiving IV piggyback antibiotics having a lower baseline systolic/diastolic blood pressure.
Conclusions: Conversion from IV piggyback to IV push administration of antibiotics in sepsis reduced time to first dose of antibiotics without negatively affecting sepsis mortality. Our study team is currently updating these numbers with more recent data and additional outcome measures such as admission to an intensive care unit (ICU) and ICU length of stay.