Background: Ceftriaxone or cefotaxime has been the drug of choice to treat spontaneous bacterial peritonitis (SBP) for many years, but little is known about microbiology, resistance rate to cephalosporines, and clinical outcomes over the last few decades. Our study aimed to describe the clinical and microbiological characteristics of culture-positive SBP at University of Kentucky Hospital.
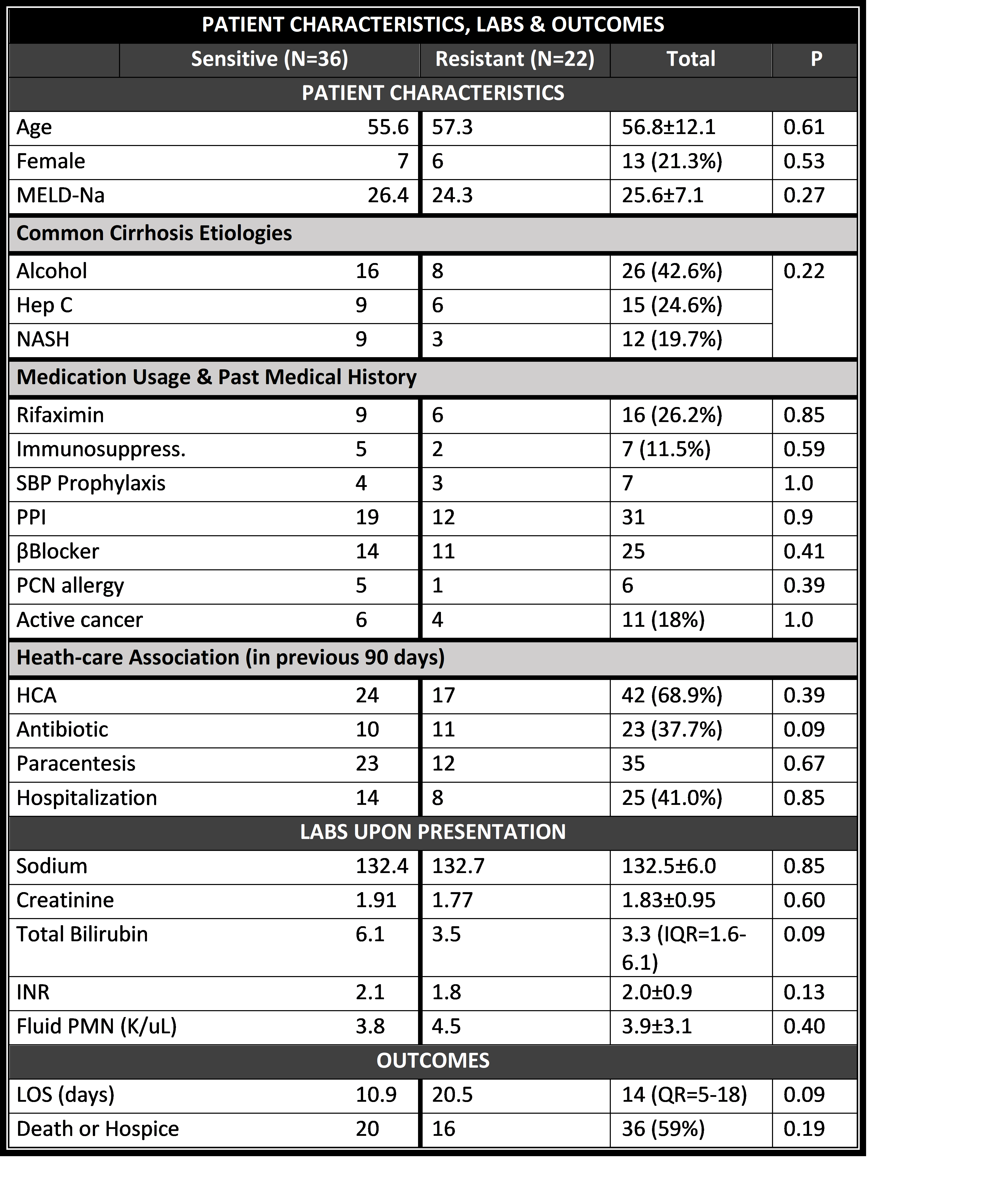
Methods: We conducted a retrospective chart review of 61 consecutive hospitalized patients who were diagnosed with culture-positive SBP at a single academic medical center. We identified 404 patients using ICD 9 and 10 codes for “spontaneous bacterial peritonitis” between 01/01/2010 and 12/31/2018. Among 98 patients who had positive fluid culture, 61 patients were included in our analysis (37 were excluded as our inclusion criteria included adult patients with no evidence of surgically treatable infection, fungal or polymicrobial infection). Descriptive analysis was performed to examine the characteristics of the patients, clinical parameters, and outcomes.
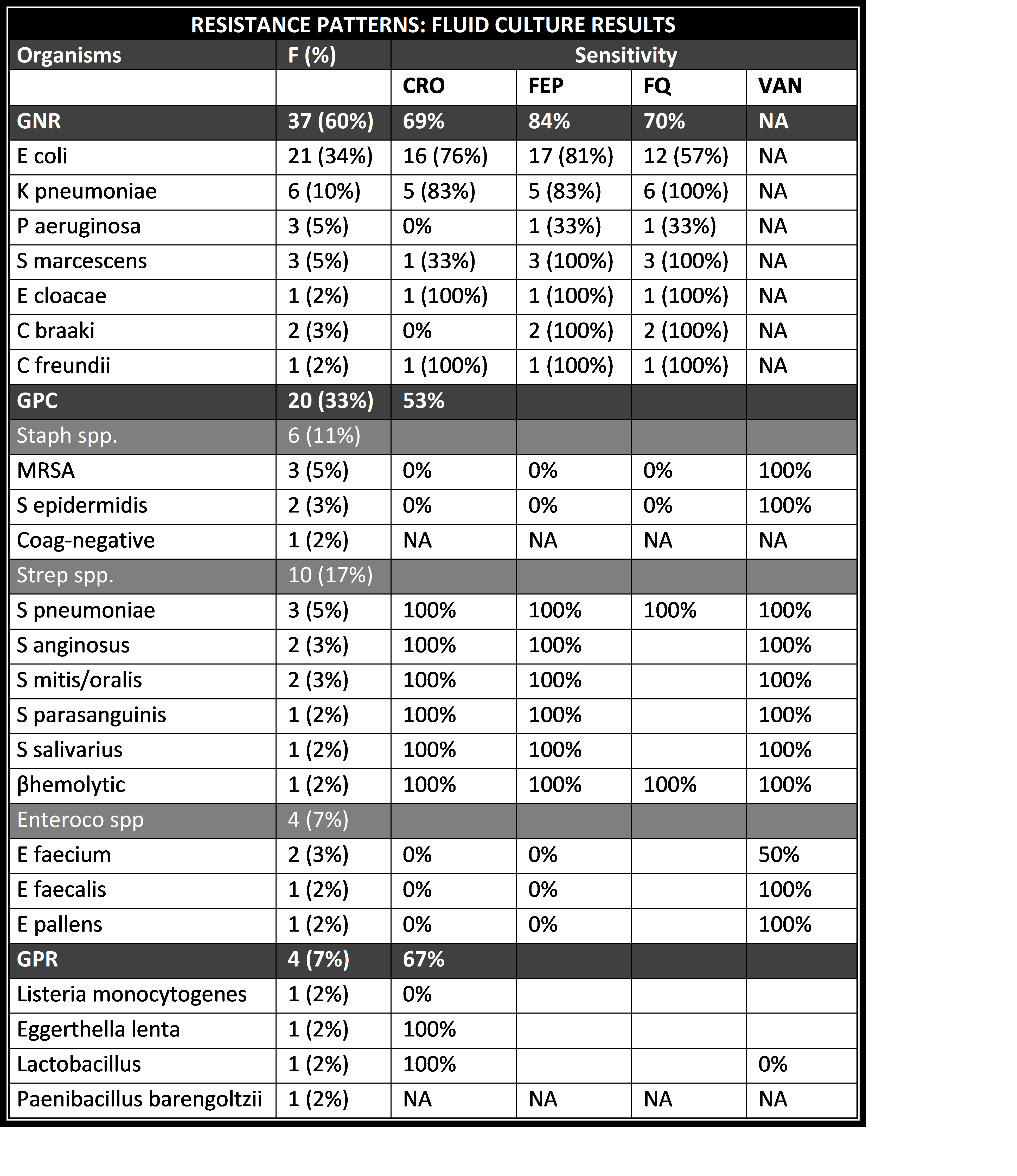
Results: Descriptive analysis showed mean age of 56.8±12.1 years, 79% of male, MELD score of 25.6±7.1, Child-Pugh score of 11.5±1.75, systolic blood pressure (BP) of 104.9±20.2 mmHg, and pulse of 95.6±17.2 bpm. Our patients had history of SBP in 15 cases (24.6%), rifaximin use in 16 (26.2%), immunosuppressant use in 7 (11.5%), end stage renal disease on hemodialysis in 3 (4.9%), active cancer in 11 (18%), and liver transplant in 1 (1.6%). In the last 90 days, they had antibiotic use in 23 (37.7%), GI bleed in 7 (11.5%), and GI procedures in 16 (26.2%). The common chief complaints included abdominal pain in 27 (44.3%), confusion in 10 (16.4%), ascites in 9 (14.8%). The common etiologies of cirrhosis were alcohol in 26 (42.6%), hepatitis C in 15 (24.6%), and NASH in 12 (19.7%). Microbiological features were as follows: Negative gram stain in 50 (82%), gram-positive cocci in 3 (4.9%), gram-negative rods in 7 (11.5%); the common organisms included 21 Escherichia coli (34%), 6 Klebsiella pneumoniae (10%), 3 Methicillin-resistant Staphylococcus aureus, 3 Streptococcus pneumoniae, 3 Pseudomonas aeruginosa, and 3 Serratia marcescens (5% respectively). 22 (36.1%,) were ceftriaxone-resistant; 20 (32.8%) had multi-drug resistance; antibiotic treatment was sensitive in 31 (50.8%); blood culture was positive in 17 (27.9%); ceftriaxone was used as the first empirical coverage in 33 (36.1%) but resistant to ceftriaxone in 10 (30%). Outcome data showed ICU stay in 27 (44.3%), median length of hospital stay of 14 days (IQR= 5-18). 36 (59.0%) had a poor outcome as 20 (32.8%) deceased and 16 (26.2%) chose hospice care during the index hospitalization.
Conclusions: Culture-positive SBP had a high mortality rate as well as a high resistance rate to ceftriaxone. Further study is needed to examine predictors of culture-positive SBP and ceftriaxone resistance that will help practitioners alter its antibiotic choice in patients with suspected SBP.