Background: Care transitions expose hospitalized patients to risks of discontinuity of care. Although various forms of care transitions have been widely studied, little is known about inter-hospital transfers (IHT, the transfer of patients between acute care hospitals). We used national Medicare data to examine the frequency of IHT and compare patient characteristics of transferred versus non-transferred non-critical care medical and surgical patients.
Methods: We performed a retrospective analysis using 2013 100% Master Beneficiary Summary and Inpatient claims files from CMS. Beneficiaries were eligible for inclusion if age ≥ 65, continuously enrolled in Medicare A and B, with an acute care hospitalization claim, excluding Medicare managed care and ESRD beneficiaries. Transferred patients were defined as those with a “transfer out” claim in their discharge status, indicating transfer to another acute care hospital. Top diagnoses at time of transfer and most common medical conditions of transferred patients were identified using ICD-9 codes of primary diagnosis and comorbid conditions at time of transfer. Patient and hospital characteristics of transferred versus non-transferred patients were compared using chi-square analyses to calculate relative risk of transfer.
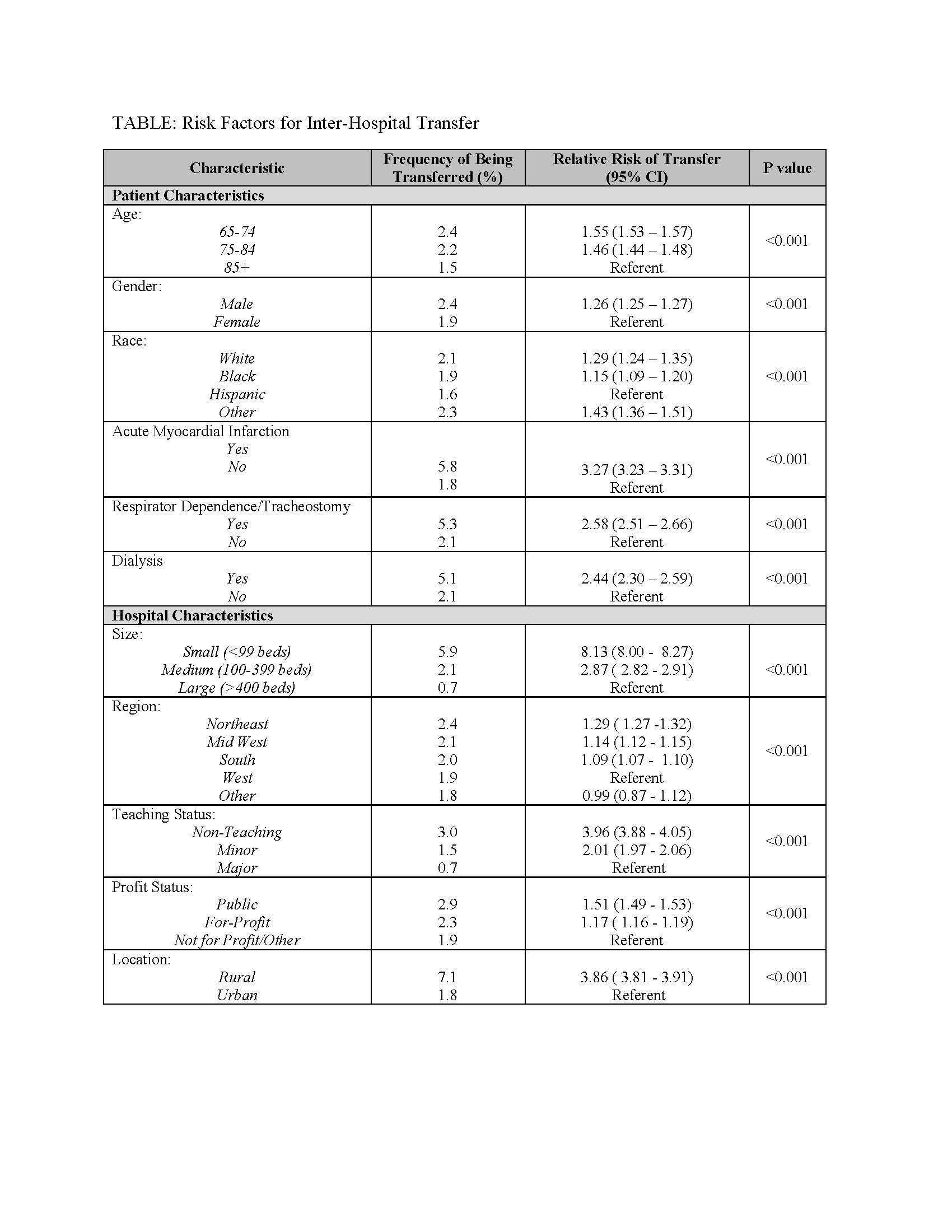
Results: Among 28 million eligible beneficiaries, 7.3 million had an acute care hospitalization. Of these, 153,779 were transferred to another acute care facility (2.1%). Among transferred patients, the top 5 primary diagnoses at time of transfer included Acute Myocardial Infarction (AMI) (10.4%), Congestive Heart Failure (CHF) (7.0%), Sepsis (6.7%), Arrhythmia (6.2%), and Pneumonia (4.5%). Comorbid conditions most commonly present in transferred patients included CHF (50.2%), renal failure (49.7%), arrhythmia (47.1%), and chronic obstructive pulmonary disease (36.9%). Younger age white men were more likely to be transferred. Small, non-teaching, rural hospitals in the northeast were more likely to transfer patients. Risk factors associated with transfer are further shown in Table 1. 30-day mortality among transferred patients was 12.6% compared with 9.6% of non-transferred patients (p<0.001).
Conclusions: To our knowledge this is the largest cohort examining IHT that has been compiled. Our data demonstrates that IHT occurs at a moderate rate nationwide, with large variation by hospital type. Patients are transferred for high acuity conditions with high frequency of serious comorbid conditions. Characteristics of transferred and non-transferred patients clearly differ. This foundational study is an important initial evaluation of this understudied patient population, and warrants further investigation to examine the benefits, harms, and safety and quality of this care transition.