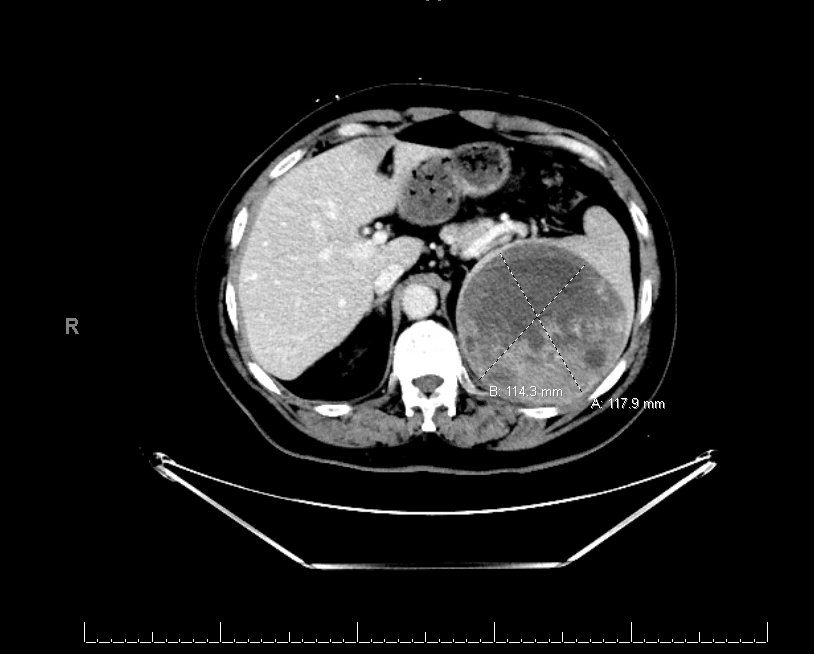
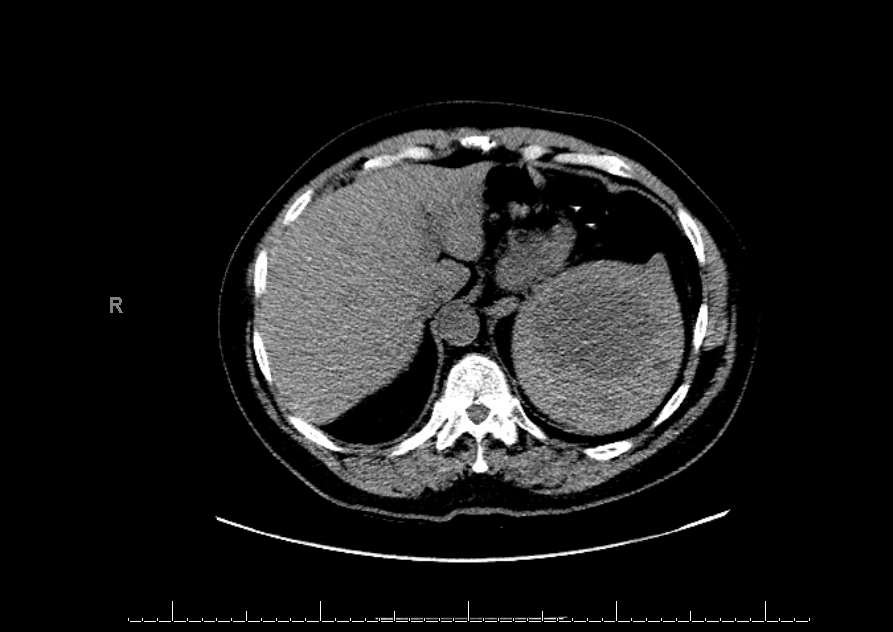
Case Presentation: A 65-year-old African American male with known comorbidities of Hypertension, coronary artery disease was brought to the hospital with a new-onset seizure. Upon presentation, vital signs were within normal limits. Physical examination noted left gaze preference, right hemiplegia, and aphasia. All labs including blood chemistries, complete blood counts, infectious workup, and urine drug screen were negative. Ct scan of the head showed left posterior mass. MRI brain showed 35 x 18 mm left parietal extra-axial enhancing mass concerning for meningioma. CT scans of chest/Abdomen/Pelvis were obtained for further metastatic workup. Interestingly his CT abdomen demonstrated a large complex partially necrotic splenic lesion measuring 12 x 12 x 12 cm with small areas of calcification. Of note, the patient did not report abdominal pain, nausea or vomiting. His abdominal examination was also unremarkable. The patient underwent left parietal craniotomy for tumor resection with histopathology showing atypical meningioma. Gastroenterology was consulted for further evaluation of the splenic mass. The patient then underwent an Endoscopic ultrasound with fine needle aspiration (FNA) which demonstrated an enlarged, mixed echogenic mass approximately 7 x 5 cm in size. Histopathology showed small lymphocytic lymphoma/Chronic lymphocytic leukemia. Due to the absence of adenopathy, cytopenia or B like symptoms, flow cytometry was also obtained which was consistent with CLL diagnosis. Given the patient was asymptomatic and there was no overt leukemia/lymphoma, the decision was made to do six monthly regular follow-ups to monitor for disease progression. Complete blood count, peripheral blood smear and repeat CT scan of the Abdomen showed stable disease at six months of follow-up.
Discussion: Chronic lymphocytic leukemia is a low-grade B- lineage lymphoid malignancy of older individuals with the heterogenic presentation. Disease course ranges from indolence to symptomatic to rapidly progressive tumor. Indolent cases are mostly diagnosed with routine blood tests revealing leukocytosis. Our case is unique in a way that our patient had no leucocytosis or symptoms despite having a splenic mass. Our case emphasizes the importance of careful evaluation of incidental findings. Even if no intervention is warranted, close follow up is necessary so that any change in disease course can be addressed promptly. The patients should be educated about the course and severity of their disease so that they could follow with their appointment on regular basis and disease progress can be monitored appropriately.
Conclusions: Advancement in technology has proven very beneficial in radiological medicine, with different modalities helping to diagnose a wide range of pathologies. Also, it has increased the number of incidentalomas which brings a challenge regarding their management. It is important to have a multidisciplinary approach to address crucial incidental findings, and appropriate follow-ups are needed to monitor the progression of the disease to avoid any catastrophic outcome