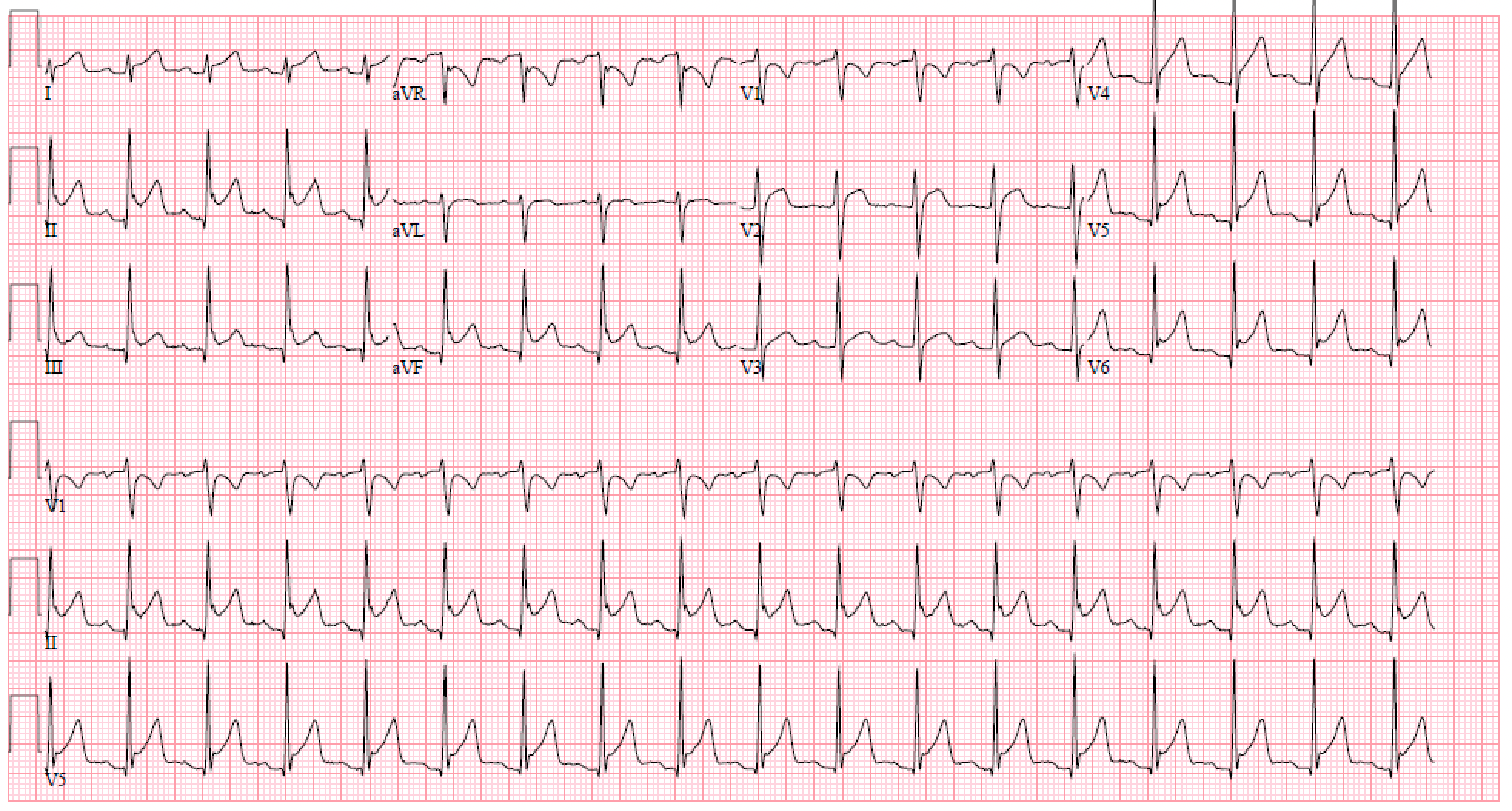
Case Presentation: A 27-year-old man with a family history of Grave’s Disease presented with acute onset pleuritic chest pain and associated shortness of breath. The patient endorsed subjective fevers and myalgias for one day prior to admission. Vital signs were significant for a heart rate of 110, otherwise unremarkable. Initial work-up showed troponin elevation to 5292.7 ng/mL, EKG revealed diffuse ST elevations and PR depression in V1 and aVR (figure 1). Left heart catheterization showed no coronary artery disease. Transthoracic echocardiogram showed right ventricular enlargement with abnormal septal motion and decreased systolic function. Left ventricular ejection fraction was 64%. Infectious workup including HIV, rapid viral panel, tuberculosis and COVID 19 testing was negative. There was no history of new medications, recent vaccinations, or international travel that would suggest a clear etiology. Further investigation into the patient’s new onset myo-pericarditis revealed thyroid-stimulating hormone (TSH) < 0.007, total T3 208 ng/dL (80-200 ng/dL), and free T4 4.6 ng/dL (0.9-1.8ng/dL). Thyroid ultrasound showed diffuse hyperemia. These findings were consistent with new onset Graves’ disease. This was confirmed with positive TSH receptor antibody testing. Cardiac MRI revealed diffuse pericardial enhancement suggestive of pericarditis without extensive myocardial involvement, although the elevated troponins were highly suggestive of some myocardial involvement. The patient was successfully managed with colchicine, ibuprofen, methimazole, and metoprolol and was ultimately discharged after complete resolution of his chest pain and tachycardia.
Discussion: We describe a case of new onset Graves’ Disease presenting as myo-pericarditis. In developed countries, 80-90% of cases of pericarditis are due to a presumed viral etiology, typically the Coxsackie viruses, Epstein-Barr virus, and Parvovirus B-19.1 Similarly, Graves’ Disease can also be triggered by viral infection, notably Epstein-Barr virus, Hepatitis C, and Parvovirus B19.2 Recent reports have described a presentation of both Graves’ Disease and pericarditis, termed thyro-pericarditis.3, 4 Some reports postulate a distinct causative relationship and shared underlying autoimmune process between Graves’ Disease and pericarditis,5 while other reports suggest that pericarditis develops from thymic hyperplasia secondary to Graves’ Disease, supported by some case reports with a grossly negative viral infectious work-up.6, 7 Given our patient’s subjective fever and myalgias, it remains possible that an underlying viral infection triggered the onset of both Graves’ Disease and pericarditis. However, given the patients family history of autoimmune disease, he had some predisposition, and his clinical presentation could represent Graves’ disease induced pericarditis.
Conclusions: We describe a rare case of thyro-pericarditis as the first presentation of new onset Graves’ disease. It remains unclear whether there is a causative relationship between our patient’s new onset Graves’ Disease and pericarditis, or if both are driven by a shared autoimmune etiology. However, it remains important for hospitalists to be aware of the relationship between pericarditis and Graves’ disease so that early thyroid testing can be performed, and concurrent thyrotoxicosis and pericarditis management can be initiated.