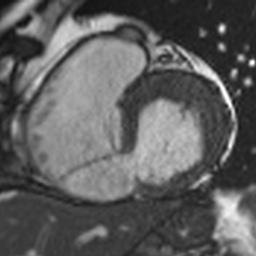
Case Presentation: An 86 year old man with hypertension, COPD, and a 100 pack year smoking history presented to the emergency department with 1 week of dyspnea and neck pain. He had a blood pressure of 104/74, heart rate 85, respiratory rate 27, and SpO2 95% on 3 liters nasal cannula. Labs were significant for Pro-BNP 12376, AST/ALT 348/342, troponin 7.39, and lactate 4.7. EKG showed normal sinus rhythm with second degree AV block Mobitz type 1 and ST depression in anterior leads. Chest x-ray showed pulmonary edema. Due to worsening dyspnea and neck pain considered to be anginal equivalents, urgent left heart catheterization (LHC) was performed which revealed a 100% right coronary artery (RCA) occlusion. Left ventriculogram showed ejection fraction 55% and pulmonary capillary wedge pressure 33 mmHg (reference range 4-12 mmHg). He was unable to be revascularized due to desaturation and dyspnea and was admitted to the ICU. In the ICU, transthoracic echocardiogram (TTE) with Doppler demonstrated a 12mm basal inferoseptal ventricular septal rupture (VSR) associated with left to right shunting that had not been visualized on LHC. Due to his age and comorbidities, he was not a candidate for surgical repair. Instead, percutaneous transcatheter septal closure (TSC) was explored. Cardiac MRI (CMR) revealed a dissected tissue flap originating from the right ventricular (RV) endocardium, consistent with intramyocardial dissection (IMD). Intra-arterial balloon pump was attempted as a bridge to TSC, however the patient could not tolerate the procedure due to agitation. He was then intubated and placed on Norepinephrine for right heart catheterization (RHC) which showed a step-up in oxygen saturation of 58% to 80% from RA to RV, Qp:Qs 2.33, and cardiac index 2.10, findings consistent with severe left to right shunting complicated by cardiogenic shock. During RHC, a wire could not be passed through the VSR due to obstruction by the myocardial flap from the IMD, preventing percutaneous repair. Ultimately, family opted to compassionately extubate the patient the following day.
Discussion: VSR, albeit rare, is a deadly consequence of myocardial infarction (MI) that has decreased in incidence from 1-3% to 0.17-0.31% with the advent of percutaneous coronary intervention (PCI) (1). Nonetheless, post-MI VSR is associated with a mortality rate of 38% for those percutaneously repaired, increasing to 88% in those with cardiogenic shock (2). While TTE is the gold standard for diagnosis, CMR can further demonstrate the extent of necrosis, and RHC helps characterize shunting with a Qp:Qs ratio >1.5 indicating a severe shunt (3, 4). This is important as repair is limited by the VSR’s anatomy, with the optimal size for TSC being < 15mm (1). Unfortunately, as in our patient, RCA and inferior infarcts are associated with larger, more serpiginous defects and more commonly result in IMD (1).
Conclusions: Our case details a rare instance of post-MI VSR and illustrates that management of hemodynamically unstable patients with structurally complicated VSR is challenging and requires clarification.