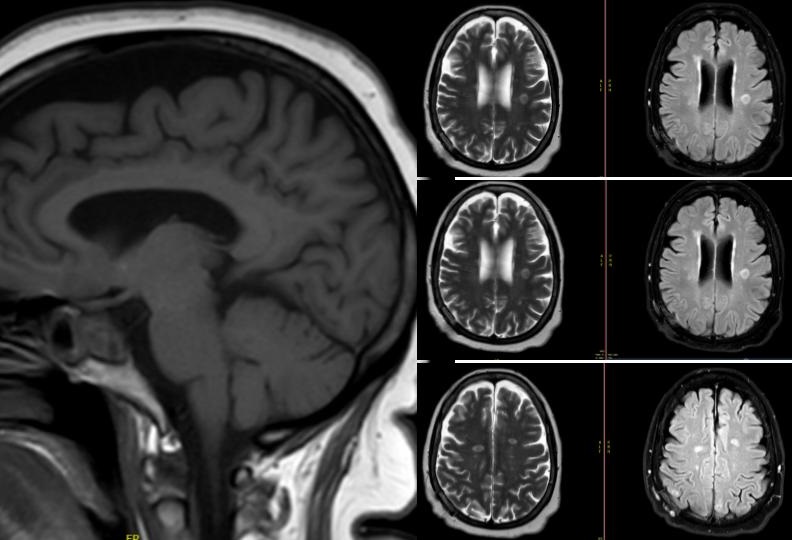
Case Presentation: In infectious disease diagnostics, Next-Generation Sequencing (NGS) is a game-changer. The test is particularly useful when regular tests are unable to pinpoint the problem, especially in healthy people with no risk factors for unusual infections. It enhances pathogen identification through genetic analysis A 55-year-old woman with sigmoid diverticulosis and recurrent urinary tract infection (UTI) presented with dizziness, dysuria, hematuria, and a fall. Vital signs and physical exam were normal. Labs showed WBC 13.5 K/uL and abnormal urinalysis. UTI treatment was started. However, her persistent dizziness prompted further investigation. A head computerized tomography (CT) scan unveiled a 2.2 x 2 x 3.3 cm suprasellar lesion. Further evaluation revealed a non-hormone-producing pituitary macroadenoma. Subsequent MRI imaging revealed 12 ring-enhancing lesions in both the infratentorial and supratentorial regions, consistent with abscesses. Empirical antibiotic therapy with ceftriaxone, metronidazole, and vancomycin was initiated. Comprehensive infectious studies and cultures were carried out on serum, urine, and cerebrospinal fluid, all of which were negative. Autoimmune and inflammatory studies were also unremarkable. Transesophageal echocardiogram did not detect any vegetations. CT scan of the spine, abdomen, and pelvis detected an unexpected colovesical fistula while eliminating the possibility of additional infection sources. Brain biopsies showed purulent lesions with negative cultures, but Streptococcus dysgalactiae was later identified through NGS 16s ribosomal RNA testing. The suspected source, a colo-vesical fistula, was surgically resected. Eight weeks of intravenous antibiotics (ceftriaxone and metronidazole) led to MRI improvement. Treatment then shifted to oral levofloxacin until the lesions completely resolved on imaging.
Discussion: S. dysgalactiae, similar to S. pyogenes, causes invasive infections, especially in immunocompromised individuals. [4,5] Severe infections often correlate with conditions like cancer (21-65%), diabetes, cirrhosis, or alcohol abuse. [2,6–8]. Compromised bowel mucosa, such as in necrotic tumors, can permit bacteria in the bloodstream, as observed in S. agalactiae endocarditis and colorectal carcinoma. [9,10]. Epidemiologic data on S. dysgalactiae is limited. This bacterium is also associated with acute pyogenic meningitis, which has a high mortality rate. [1,2] We present a case of an immunocompetent patient with no identifiable risk factors (e.g., animal exposure, travel, housing) who was unexpectedly diagnosed with brain abscesses during a pituitary adenoma evaluation. Brain abscess diagnosis typically relies on CSF microbiological cultures, but this approach can be inconclusive in a significant percentage of cases (20-50%). Our comprehensive infectious workup ruled out endocarditis, which is associated with high mortality in cases of Group G Streptococcus meningitis. In this case, the infection likely originated from the blood via a colo-vesical fistula, rather than from local contamination related to an epidural infection. To ensure proper antibiotic treatment, NGS played a crucial role in identifying the specific pathogen, S. dysgalactiae.
Conclusions: Prompt diagnosis, surgery, and precise antibiotics are crucial for treating Streptococcus dysgalactiae brain abscesses, regardless of the patient’s immunity. NGS may be necessary for diagnosis when standard tests are less sensitive.