Background: The process by which patients are admitted to the inpatient setting after evaluation in the emergency department (ED) is a critical component of their care transition. Striking the proper balance between the speed of the process and the quality of the communication is paramount to optimizing workflows and ensuring patient safety. At our institution, a 750-bed quaternary care academic medical center located in New York, our hospitalist team receives over 50 admissions per day, with volume increasing year-over-year. Each shift, one hospitalist, termed the “Hospitalist-In-Charge (HIC)”, is assigned to lead this process, serving as the primary contact for our EM colleagues. The mode of communication between teams has historically been via pagers and landline phone calls, with manual transcription of information, external to our EMR. As the number of admission requests have increased over time, the bandwidth of the HIC has decreased, resulting in admission delays and low physician satisfaction.
Purpose: An interdisciplinary collaborative was created to redesign our ED admissions process, with the goal of eliminating the need for pager-based communication, improving closed-loop communication, and providing teams with automated and pertinent information directly pulled from our EMR via an external, HIPAA-compliant platform to improve operations and streamline the process.
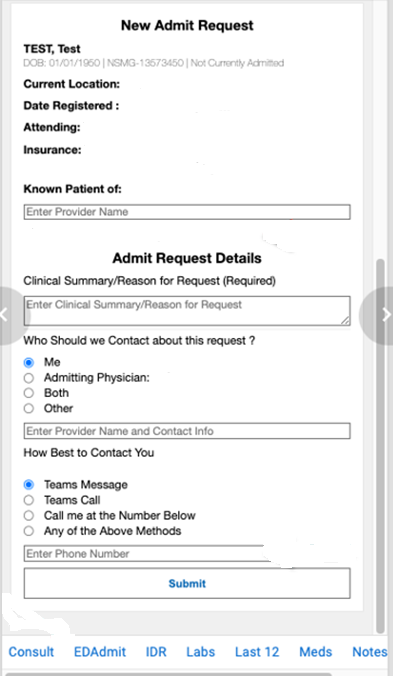
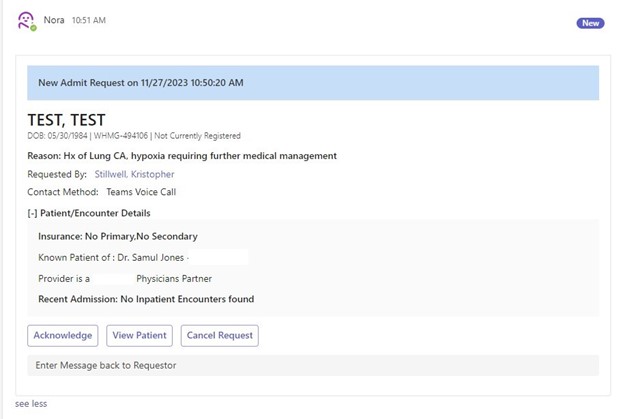
Description: Our collaborative of hospitalist, EM, and IT leaders began to in early 2023 to determine how best to redesign our admission process. A mutual desire to transition the initial request for admission from a pager-based modality to one that was primarily chat-based was identified. Leveraging Nora, a Microsoft chatbot with the ability to pull patient-specific clinical information into our Microsoft Teams platform via “patient cards”, our teams were able to develop a workflow by which initial admission requests are submitted and reviewed. Nora can be accessed at workstations or via mobile device. The card was customized to auto-populate key information (demographics, primary care physician, provider contact information, etc.) that was available in our EMR, as well as the ability to free-text pertinent clinical information. Once the request is posted by the EM provider to the channel, the HIC can acknowledge receipt, review the case, and then connect directly with the requesting EM provider via Microsoft Teams to finalize the warm handoff. When a request is acknowledged or completed, our EM teams receive automated closed-loop communication via the chat platform.
Conclusions: By transitioning to an electronic means of communication, automating the receipt of key demographic and clinical information that are critical to the admissions process, our HICs have noted a significant decrease in the volume of pages received, as well as amount of time spent on the phone discussing cases for admission. Additionally, we believe that the quality of the transitions of care has also improved; as exchanged information is automated, there is a decreased chance for transcription errors, and the time saved during these interactions by upstreaming receipt of information translates into higher quality chart reviews. Both our EM and hospitalist teams have reported increased satisfaction in the process with enhanced response times. With the success of this innovation, we look forward to leveraging the platform to assist with standardizing other consult-related processes between teams at our institution.