Background: Improving the quality and safety of the care provided is the some of the most essential and critical work done in hospitals today. In the current system of health care education, health care professionals are often trained on improvement methodology. Several methodologies are provided as improvement frameworks in our health care professional schools around the nation. Contrasting methodology education produces multidisciplinary teams often speaking “different languages” when engaging in improvement work. The consequence is unproductive teams or professions approaching this work in silos. As hospitalists, we serve as division leaders, hospital leaders and medical educators at our respective institutions. We are uniquely positioned to assist in developing a framework which aligns the methodology utilized by all team members and disseminating this methodology to our clinical care teams, hospital medicine divisions, trainees, and students.
Purpose: Under the direction of hospital administration, we assisted in developing and disseminating a framework that incorporated the different methodology utilized by our team members to improve patient safety and quality at our institution.
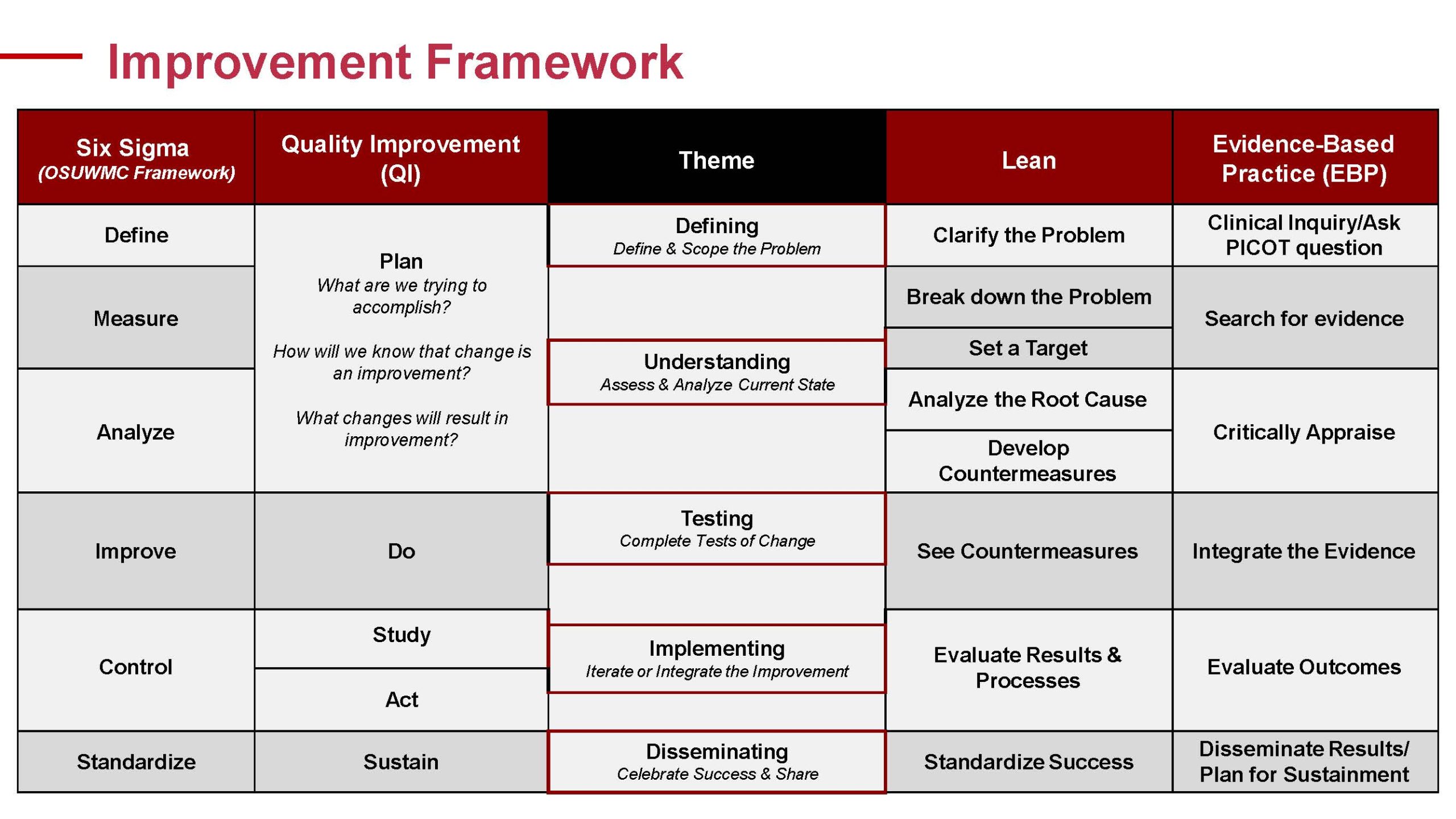
Description: At our academic medical center, improvement work was approached utilizing several methodologies. Faculty physicians and GME training programs utilized either The Improvement Model or DMAIC (Define, Measure, Analyze, Improve, Control, a subset of Six Sigma). Nursing preferred the Evidence Based Practice Model taught by the Fuld National Institute. Therapy typically utilized The Improvement Model and Implementation Science. Finally, our Process Improvement Team utilized Lean and DMAIC/Six Sigma exclusively. Multidisciplinary teams approaching improvement work often utilized different methodologies across the institution. Teams were not high functioning due to differing levels of training in the specific improvement method being utilized by the team. Led by a hospital administrator, we developed a framework to showcase how the methodologies aligned and could be utilized together to improve care (Figure 1). Utilizing this framework, the medical center developed regular monthly development sessions for local leadership teams to aid in incorporating this framework into their improvement work. Hospitalists serve on these teams as medical directors. To continue dissemination and incorporation of this framework into improvement work, hospitalists have begun to utilize this framework in GME quality improvement education as well as required Hospital Medicine faculty development for new faculty. To strengthen the education provided on the framework, we consistently utilize multi-disciplinary experts in each model to provide the education. This reinforces the importance of multidisciplinary teams in improvement work as well as allowing the methodology experts to provide the education.
Conclusions: Improvement work is imperative in improving the quality and safety of care delivery. High functioning teams utilize consistent methodology in improvement work. We have developed a framework to incorporate several methodologies taught by health care professional schools. We suspect this framework will accelerate our institution’s ability to elevate and advance the quality and safety of the care we provide. Next steps are analyzing improvement work outcomes as a measure of success of our framework and consider incorporation of this framework into multidisciplinary health sciences education.