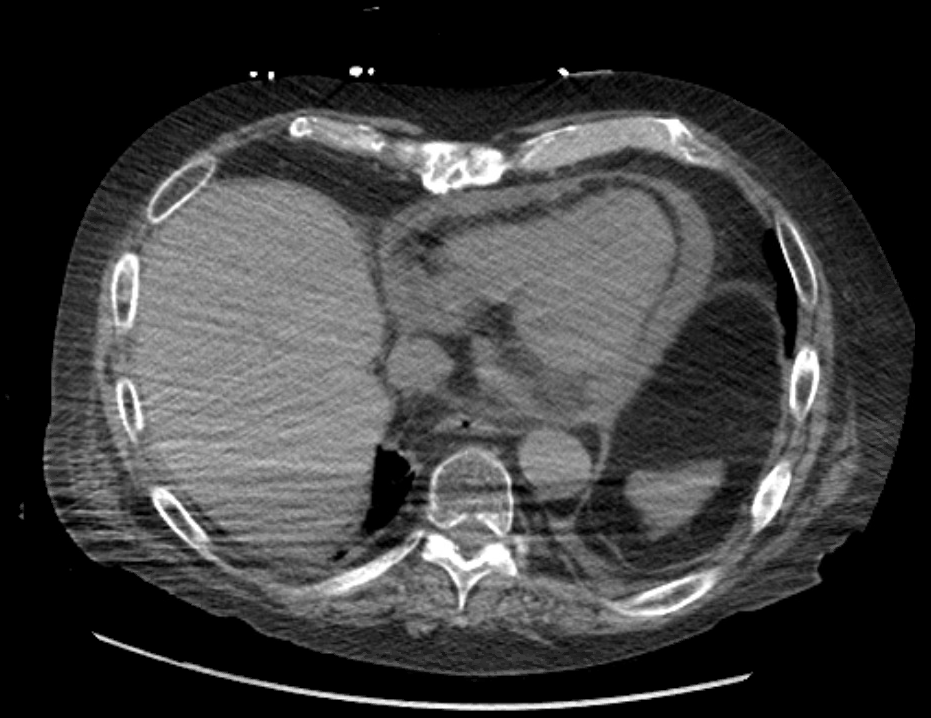
Case Presentation: A 73-year-old man with a history of atrial fibrillation on apixaban and panhypopituitarism secondary to resection of a pituitary adenoma in the 1980s presented to our hospital for chest pain. His recent history is notable for recurrent cystitis and Clostridium difficile infections requiring stress-doses of glucocorticoids; his endocrinologist had been attempting to taper his steroid doses but the patient had been resistant to decrease below 20 mg prednisone daily due to profound fatigue with dose decreases. On admission his troponin was 1.7 and his EKG showed 1 mm ST-segment elevations in leads I and aVL concerning for ST-elevation myocardial infarction. He was loaded with aspirin and ticagrelor and taken emergently to the cardiac catheterization lab where he was not found to have obstructive coronary artery disease. He was admitted for further workup of presumed myopericarditis. Stress dose steroids were started to treat his myopericarditis and his home apixaban was continued. On the evening of his first hospital day he acutely developed abdominal pain, chest pain, and encephalopathy. He was hypotensive ultimately requiring vasopressors. A CT abdomen/pelvis did not show acute abdominal pathology but did show a new pericardial effusion (Fig 1) that was not present on a transthoracic echocardiogram obtained earlier in the day. A bedside echocardiogram again showed a small pericardial effusion with early diastolic collapse of the right atrium and right ventricle consistent with cardiac tamponade physiology. An emergent pericardiocentesis was performed; 500 cc of serosanguinous fluid were removed with immediate resolution of shock. On hospital day #5, culture of pericardial fluid was found to be growing Nocardia nova. He was started on imipenem and amikacin without recurrence of his pericardial effusion. Unfortunately, his mental status failed to improve and his family felt it was not within his goals of care to search for Nocardia infection of the central nervous system with an MRI of his brain. He was ultimately transferred to inpatient hospice, where he died peacefully ten days after admission.
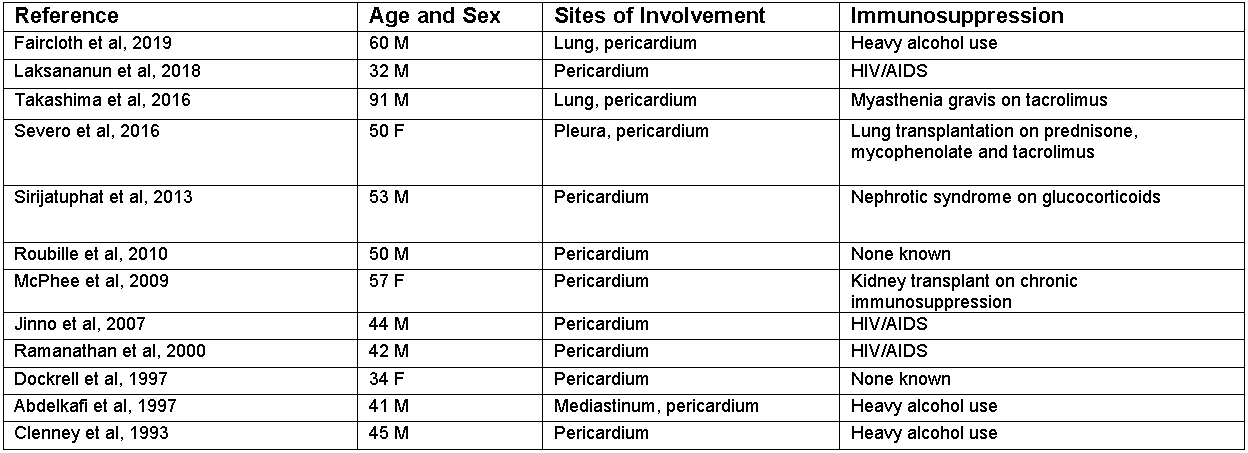
Discussion: Nocardia myopericarditis is a rare entity with few reported cases in the literature. A survey of reported cases (Fig 2) demonstrates that the conditions that convey the most risk for Nocardia pericarditis are (1) use of immunosuppressive medications (2) HIV/AIDS and (3) heavy alcohol use. The right clinical context should prompt workup for Nocardia pericarditis, especially because appropriate treatment requires a tailored antibiotic approach. There is widespread recognition that antibiotic prophylaxis for opportunistic infection such as Pneumocystis jirovecii should be considered in patients with rheumatologic diseases immunosuppressed with high-dose glucocorticoids. Our patient, although initially started on replacement doses of steroids for panhypopituitarism, had been reluctant to taper below 20 mg of prednisone daily. It is important to recognize the risks of chronic supraphysiologic doses of glucocorticoids and to discuss antibiotic prophylaxis if warranted.
Conclusions: Patients on high-dose glucocorticoids warrant consideration of prophylactic antibiotics regardless of underlying disease. Nocardia myopericarditis causing tamponade is a rare entity that, in this instance, may have been prevented with trimethoprim-sulfamethoxazole prophylaxis.