Background: Telemetry is an essential tool for real-time monitoring of the heart rhythm and QRS morphology of a patient. American College of Cardiology and American Heart Association had published their respective practice standards for in-hospital cardiac monitoring for the detection of cardiac arrhythmias. Nonetheless, these recommendations were mostly based on expert opinions which focused almost exclusively on cardiac diagnoses. Recent studies had shown a rising trend of telemetry use in non-critical care setting for non-cardiac related diagnoses due to fear of clinical deterioration and need for closer monitoring. This practice had led to overdoing of telemetry monitoring. We sought to determine the utilization patterns of telemetry in non-cardiac related diagnoses in our hospital.
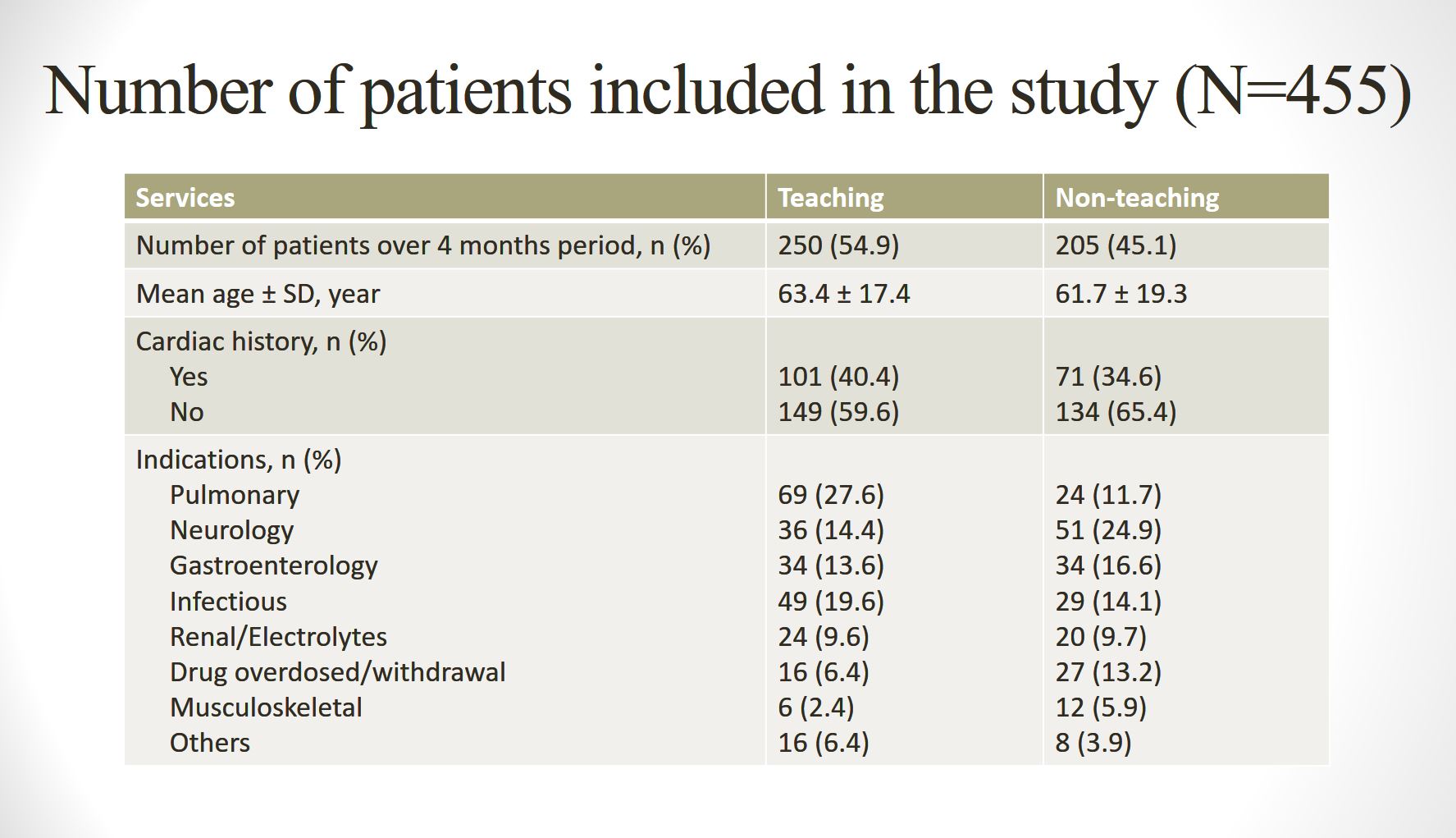
Methods: A retrospective chart review was performed on a total of 735 patients who were admitted to non-critical care bed over 4 months period (March 2017–June 2017). Inclusion criteria: Age ≥18, non-critical care beds, medicine service, at least 1 day of telemetry monitoring. Exclusion criteria: Patient with primary cardiac diagnoses or complaints. Patient records were reviewed and assessed for the appropriate use of telemetry monitoring at admission or transferred to the non-critical care bed based on our institution guideline, number of clinically significant arrhythmias, outcomes related to telemetry events, number of days that warrant a telemetry monitoring (indicated days), number of non-indicated days and the estimated financial burdens of non-indicated days, .
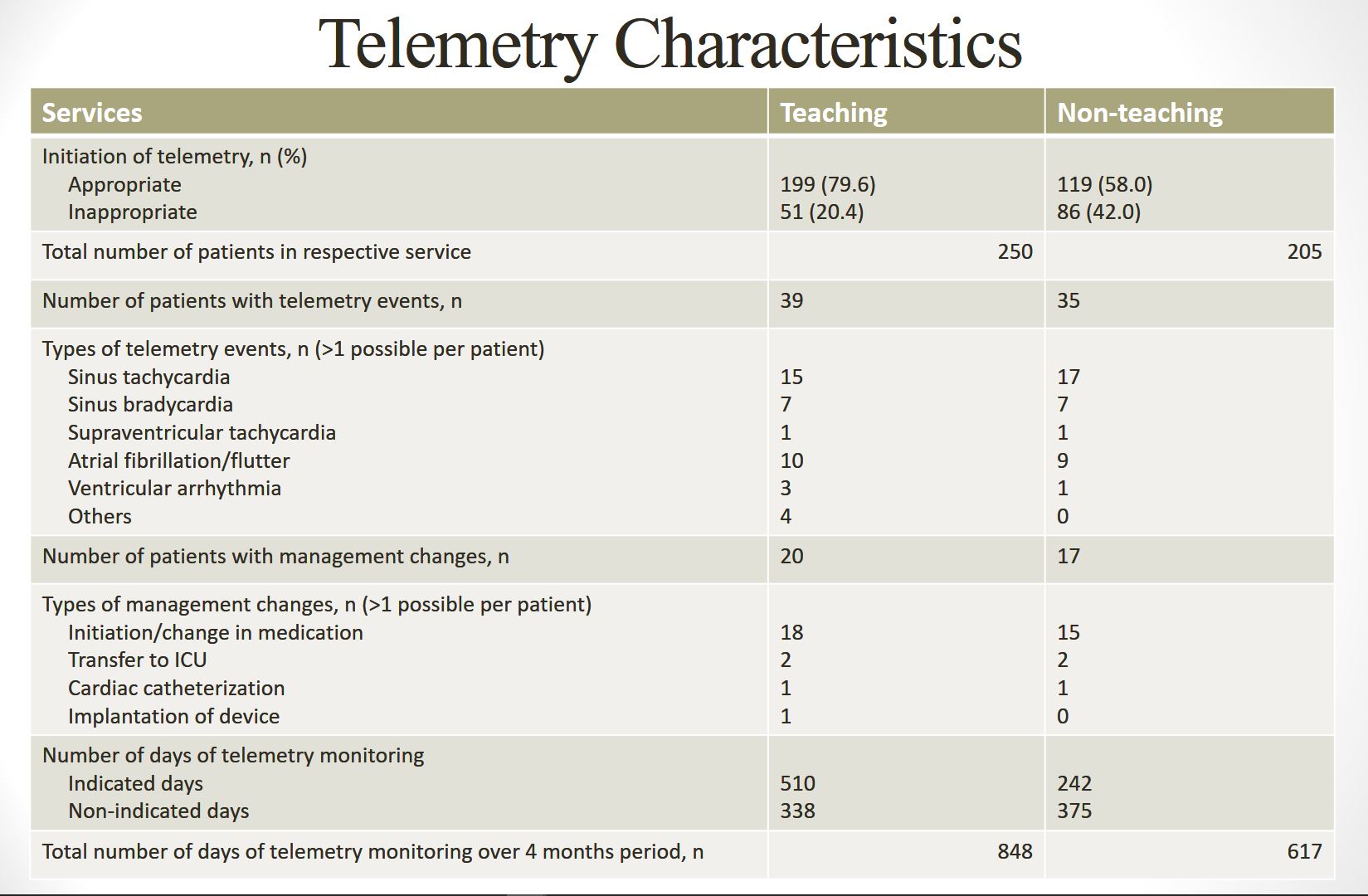
Results: Out of 735 patients, 455 patients were admitted to telemetry bed for non-cardiac related diagnoses over 4 months period. 30.1% (137/455) had inappropriate initiation of telemetry monitoring. Majority of them, 62.2% (283/455), had no known cardiac history. Clinically significant arrhythmias occurred in 16.3% (74/455) of the monitored patients, with only 8.1% (37/455) had management changes related to the telemetry events. Overall, the total number of patient days of telemetry monitoring over 4 consecutive months was 1465. On subgroup analysis by service, teaching service: 510 (60.1%) indicated days and 338 (39.9%) non-indicated days, whereas non-teaching service: 242 (39.2%) indicated days and 375 (60.8%) non-indicated days. No death event was reported in the non-indicated days. The estimated cost difference between telemetry ($7533) and medicine-surgery ($4727) bed per patient per night at our hospital was $7533 – $4727 = $2806. This was translated to a total waste of $2806 x 338 = $948,428 (teaching service) vs $2806 x 375 = $1,052,250 (non-teaching service) in non-indicated days over the 4 months period.
Conclusions: In our study, we found that most of the time physicians failed to discontinue the telemetry monitoring in a timely manner. We need to do a better job at discontinuing telemetry monitoring in non-cardiac related diagnoses to provide a cost-effective care for our patients.