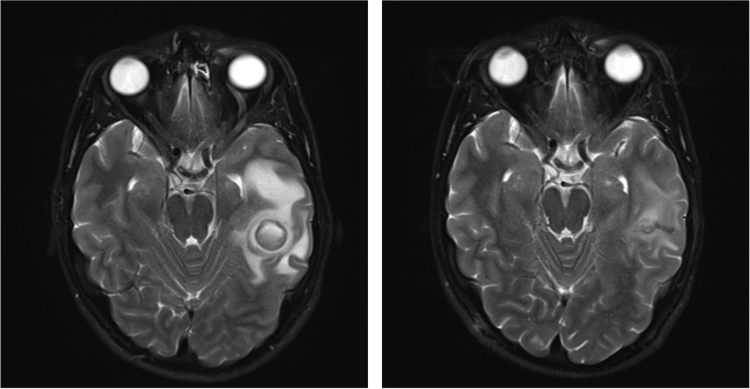
Case Presentation: A 23-year-old male was transferred to a tertiary medical center for abnormal CT head imaging after presenting with 1 week of left-sided headache. He reported that his headache was waking him from sleep and was associated with morning vomiting. He denied fevers, chills, cough, or weight loss. His neurological exam was unremarkable, as were heart and lung exams. There was no evidence of lymphadenopathy. Lab studies, including a BMP and CBC, were normal. An MRI brain demonstrated a 2.2 cm ring-enhancing lesion in the left temporal lobe with surrounding vasogenic edema, concerning for abscess versus malignancy. On further history, the patient denied IV drug use. He was sexually active with his girlfriend, always using condoms. He had never left the country. He had occasionally fished in freshwater but otherwise reported minimal outdoor exposure. He worked in heating, ventilation, and air conditioning and described exposure to dead animals and molds. There was no family history of brain cancer. Additional testing included a negative HIV Ab/Ag screen. The patient went to the OR on Hospital Day #3 for biopsy. The mass was identified as an abscess with 10cc purulent fluid drained. Initial stains described a gram positive, partially acid-fast beaded rod, confirmed by partial 16S rRNA gene sequencing to be N. farcinica. The patient was started on IV meropenem and oral linezolid, the latter chosen because of his sulfa allergy. The organism was eventually shown to have only intermediate susceptibility to meropenem, and the patient was transitioned to linezolid monotherapy. Upon identification of the abscess etiology, the patient underwent CT chest, abdomen, and pelvis for staging, notable only for a right upper lobe 1.1 cm pulmonary lesion. There were no other signs of local or remote infection. We have now been following the patient for twelve weeks. Follow-up MRI has demonstrated interval decrease in the size of the abscess and associated edema. He denies any persistent headaches.
Discussion: This report describes the successful treatment of an intracranial N. farcinica abscess with surgical drainage and linezolid monotherapy. Notably, N. farcinica abscesses are uncommon, accounting for only 2% of all cerebral abscesses [1]. The organism, though, is clinically aggressive with studies documenting a mortality rate as high as 20% in the immunocompetent and 55% in the immunocompromised [1]. Our case highlights the importance of early organism identification and aggressive therapy, particularly given the known pathogenicity and resistance to multiple antimicrobial agents [2-3]. Empiric treatment of cerebral nocardiosis often includes the use of a combination of TMP/SMX, amikacin, and imipenem-cilastatin [3-4]. This is one of the first reports documenting a good functional outcome with linezolid monotherapy. We suspect our patient acquired N. farcinica via inhalation as a result of his occupation. His pulmonary nodule is believed to represent the primary site of infection, with dissemination to the brain postulated via a pulmonary AV malformation. This conclusion underscores the importance of a detailed history, which may reveal risk factors for atypical infections that might not otherwise be suspected.
Conclusions: Solitary N. farcinica brain abscesses in immunocompetent adults can be treated successfully with surgical drainage and oral linezolid monotherapy. The diagnosis demands a high index of suspicion regardless of patient immune status and should prompt an investigation for atypical risk factors.