Background: To address bed capacity concerns related to the COVID-19 pandemic, the Centers for Medicare and Medicaid Services (CMS) waived the certificate of medical necessity for oxygen claims, allowing for reimbursement for oxygen prescribed for patients upon hospital discharge with COVID-19 respiratory illness. This reimbursement allows providers to discharge patients with COVID-19 respiratory illness still on oxygen, yet the clinical and financial impacts of this policy shift are unknown. We created a remote patient monitoring (RPM) program for inpatients with COVID-19 respiratory illness still on oxygen that includes post-discharge remote monitoring of symptoms along with biometric data. Goals of this program include: (1) promote early hospital discharge to alleviate hospital bed capacity constraints (2) provide ongoing post-discharge monitoring of symptoms and biometric data for identification of clinical decompensation and escalation, and (3) ensure a safe transition back to the outpatient provider.
Methods: This prospective observational study from November 2021 to March 2022 examines the clinical and financial impacts of our RPM pilot in conjunction with CMS’s policy shift. Inclusion criteria include patients with COVID-19 with an oxygen requirement of less than or equal to 4 liters per minute with evidence of stable oxygenation for at least 24 hours. On discharge, enrolled patients are provided a pulse oximetry device and data transmission hub. For the following 16 days, an RPM nurse performs twice daily touch points to obtain symptoms using a validated tool and biometric data. In instances of clinical improvement, the nurse follows criteria to wean oxygen. When symptoms or biometric data suggest potential clinical decompensation, there is escalation to a hospitalist via a virtual visit. Outcome measures include the number of days post-discharge until discontinuation of oxygen which represents hospital days saved, proportion of patients with decompensation requiring escalation, percent readmissions, and percent of patients successfully transitioned back to their outpatient provider.
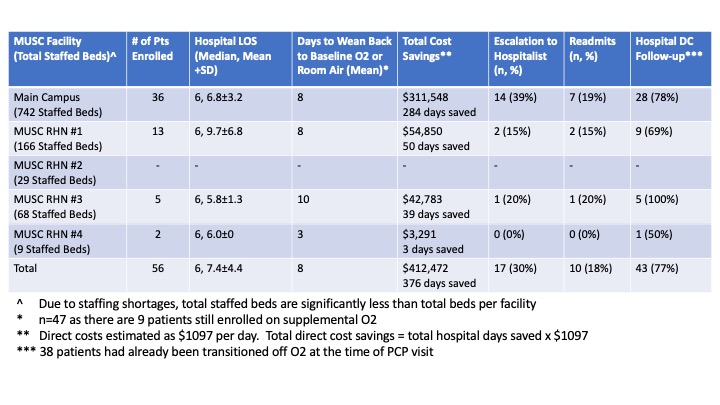
Results: Of the 56 patients enrolled in our pilot, the mean number of days post-discharge a patient remained on oxygen was 8 and the total number of days required to wean oxygen back to baseline was 376. This represents 376 hospital days saved as a result of CMS waiving the certificate of medical necessity for oxygen claims during the COVID-19 pandemic. 17 patients (30%) required escalation to the hospitalist and there were 10 readmissions (18%) (Table 1). 43 patients (77%) attended their 14-day hospital discharge follow-up appointment with 38 patients (88%) already successfully transitioned off oxygen at the time of the appointment. Given a total of 376 hospital days saved, we estimate 50 additional patients were able to be transferred into our hospitals based on an average length of stay of 7.4 days. We have attempted to estimate the cost savings associated with the CMS policy shift by calculating inpatient direct cost per day. Our finance department estimates direct costs of $1097 per day. Given a total of 376 hospital days saved, we estimate a total direct cost savings of $412,472.
Conclusions: A COVID-19 post-discharge RPM pilot, in conjunction with CMS’s decision to waive the certificate of medical necessity for oxygen claims, provides an opportunity to alleviate hospital bed capacity constraints, promote early discharges, and promote safe transitions of care.