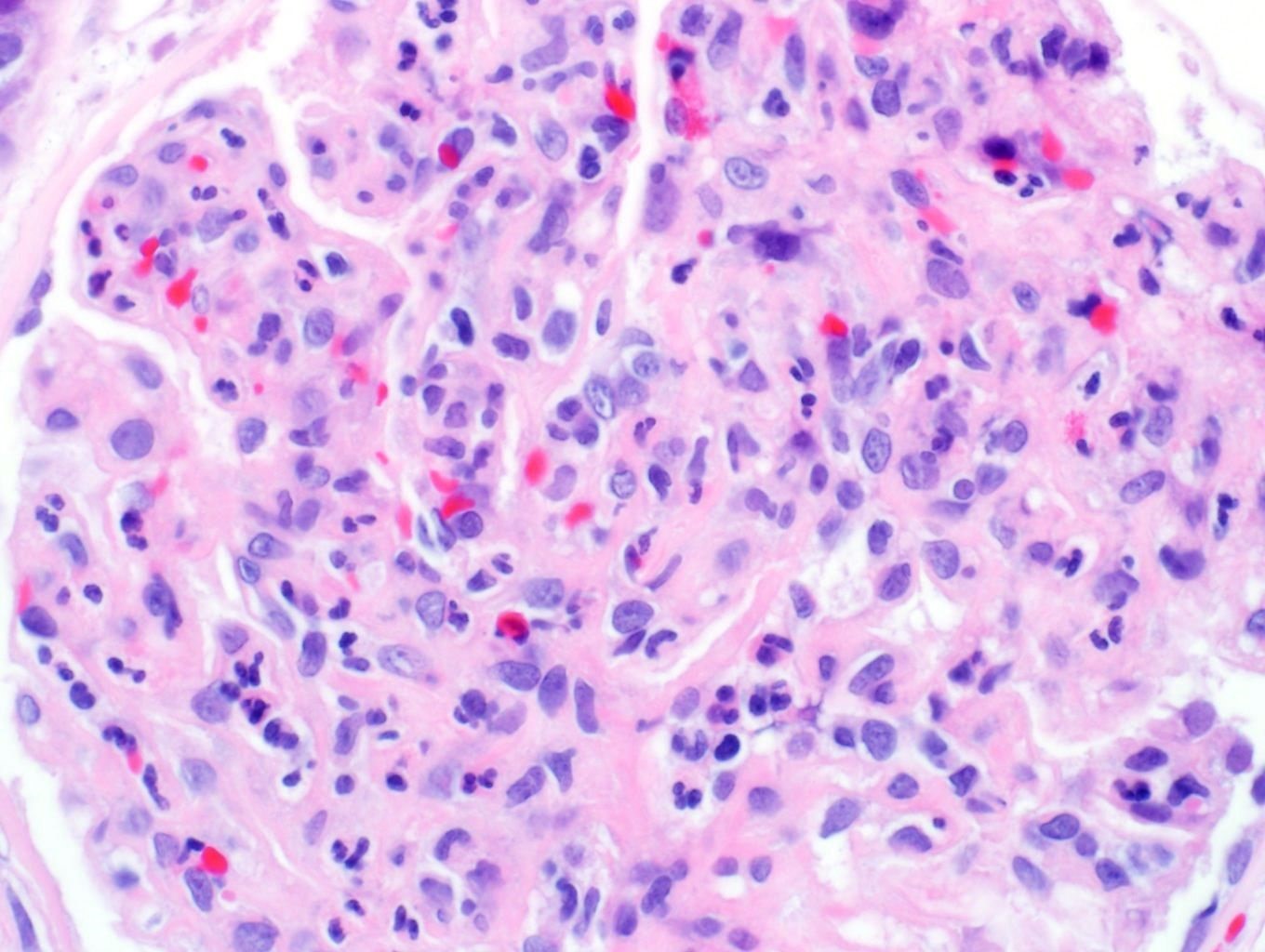
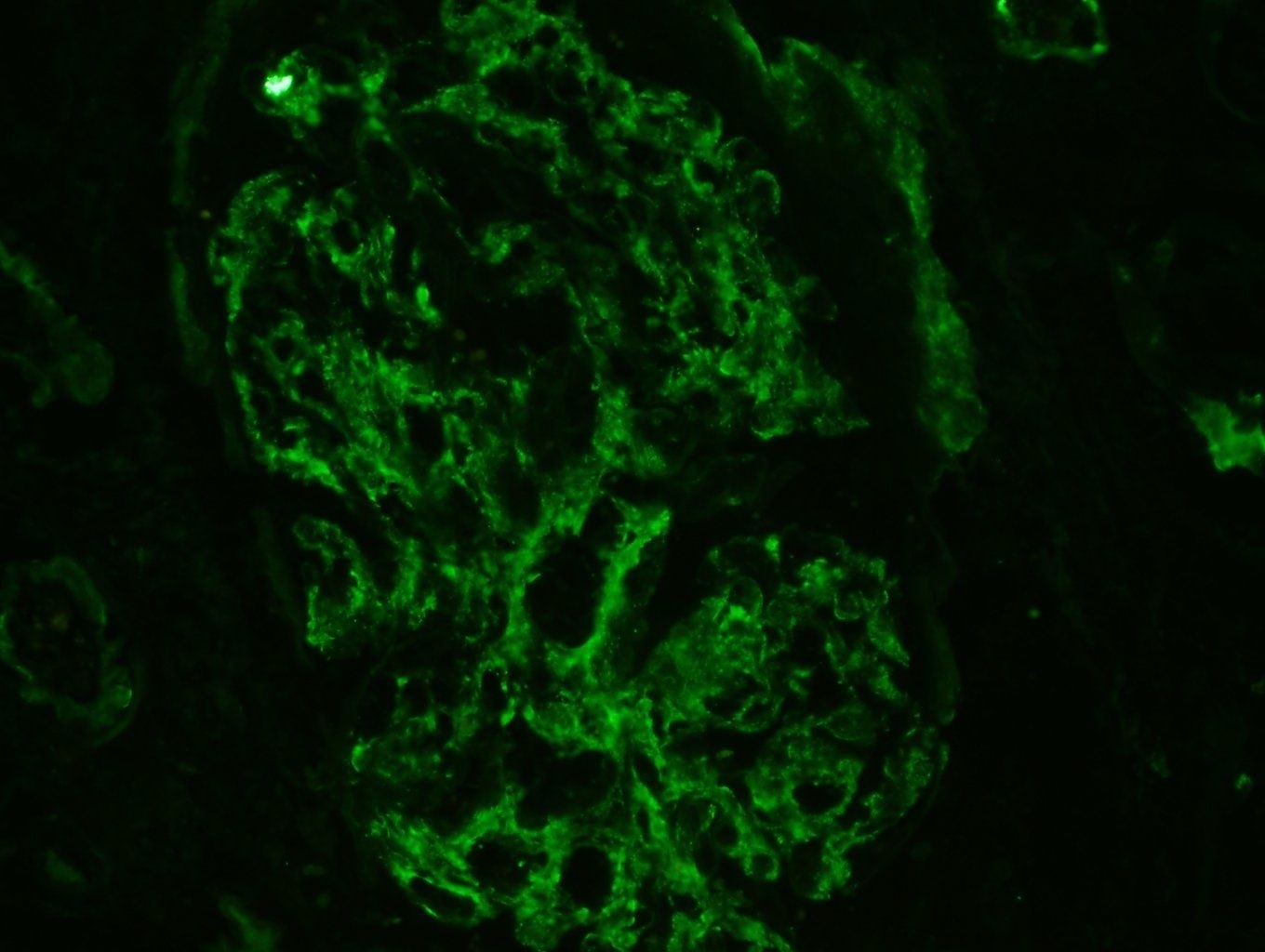
Case Presentation: A 50-year-old male with a past medical history of type 2 diabetes mellitus presented with gangrene of his left foot. The foot was erythematous with pustular eruptions. His symptoms included fevers, chills, and the inability to move his fourth and fifth digits. He was afebrile, with a leukocytosis of 19.6, erythrocyte sedimentation rate of 98, C-reactive protein of 31, complement 3 (C3) of 10, hemoglobin A1c of 9.3, and serum creatinine of 1.04. He was started on piperacillin and tazobactam and emergently taken to the operating room for debridement and subsequent amputation. A biopsy revealed osteomyelitis with gangrenous necrosis and wound cultures positive for Streptococcus constellatus. Over the following days he developed renal insufficiency with worsening hypertension. A urinalysis revealed dysmorphic red blood cells, pyuria, trace leukocyte esterase, and no nitrites. Hepatitis panel, HIV, cryoglobulins, anti-nuclear antibodies, and anti-neutrophil cytoplasmic antibodies were negative. His creatinine peaked 2 weeks after admission at 8.04. He was started on hemodialysis and a renal biopsy was done. Pathology was significant for hypercellular glomeruli without crescents or fibrinoid necrosis, granular C3 capillary and mesangial staining, and subepithelial deposits with severe podocyte foot process effacement. He was treated with surgical debridement, 6 weeks of antibiotics, and 2 weeks of hemodialysis. Three months after presentation his creatinine recovered to 1.36.
Discussion: S. milleri remains unfamiliar to many physicians regarding its classification, hindering detailed investigation and diagnosis of infections. The S. milleri group includes S. anginosus, S. constellatus, and S. intermedius. Infections associated with this group of organisms include bacteremia, oral abscesses, pneumonia, intra-abdominal infections, endocarditis, necrotizing fasciitis, and CNS infections, with complications occurring due to the organisms’ pyogenic nature. The incidence of S. milleri infections has been difficult to obtain but has been reported as 0.14 per 100,000. Cases and outbreaks of glomerulonephritis secondary to S. constellatus have been reported dating to the 1960s. More recently, animal models have demonstrated non-group A streptococcus strains may cause glomerulonephritis. S. anginosus has been reported to harbor nephritogenic antigens in animal models, suggesting a possible mechanism. Most often, acute glomerulonephritis is associated with the streptococcal species S. pyogenes rather than with the streptococcal species S. milleri group. Very few reports of such cases exist.
Conclusions: This case illustrates the one of the few reports of biopsy proven PIGN from osteomyelitis secondary to S. milleri. Hospitalists should have a high suspicion for PIGN in someone with an S. milleri infection and worsening kidney function.