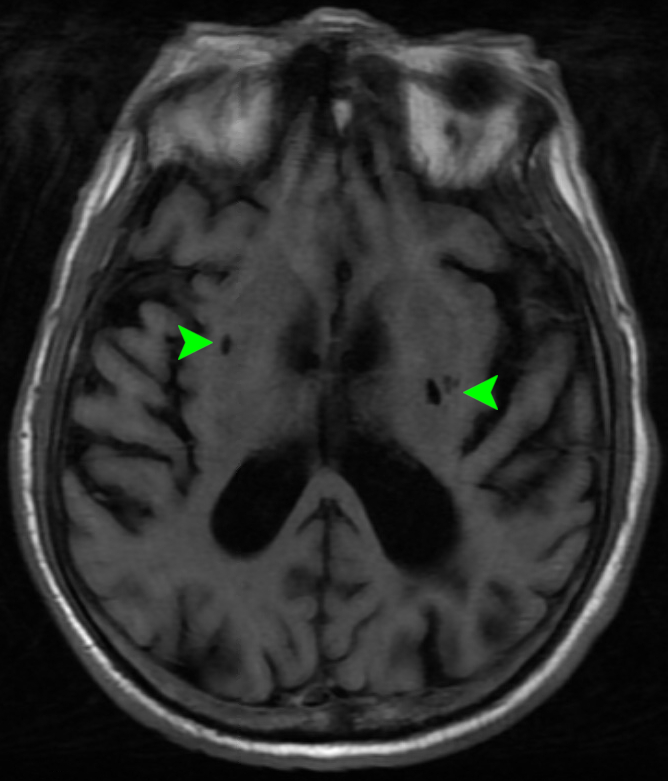
Case Presentation: A 79-year-old male with type 2 diabetes mellitus presented after being found down by a neighbor. Patient reported generalized fatigue. On exam, he was not alert or oriented, but otherwise had a non-focal neurological exam. Glucose was 742 mg/dL, bicarb 15 mmol/L, anion gap 22.8 mmol/L, and beta-hydroxybutyrate 3.92 mmol/L. CT head was negative for acute findings, but notable for chronic infarcts at multiple lobes including bilateral basal ganglia. He was admitted on an insulin drip for DKA/HHS. HbA1c was 14.3%. On day 2, the patient’s mental status improved, glucose level was 300 mg/dL, anion gap resolved, and he was transitioned to injectable insulin. On day 3, he developed high amplitude, non-rhythmic, asymmetric chorea/ballismus movements in bilateral upper and lower extremities. He was alert and aware during these bursts of involuntary movements, and expressed distress that the movements were not suppressible. MRI brain showed the previously known chronic lacunar infarcts in the basal ganglia and no acute changes [Image 1]. EEG was negative for seizure activity. Chorea Hyperglycemia Basal Ganglia Syndrome (C-H-BG) was suspected. With further optimization of the patient’s glycemia using short and long-acting insulin, he had complete resolution of his chorea within 2 days.
Discussion: Diabetes can lead to a myriad of neurological disorders, including hyperglycemia-induced involuntary movement (HIIM) disorders in patients with long-standing uncontrolled diabetes. C-H-BG syndrome is a manifestation of HIIM. Proposed mechanisms of basal ganglia dysfunction in hyperglycemic and hyperosmolar states include the shift to the anaerobic pathway in cellular metabolism resulting in the depletion of GABA, and hyperviscosity in the vasculature leading to disruptions at the blood-brain barrier [1].C-H-BG syndrome has characteristic MRI findings of T1 hyperintensity in the basal ganglia [2]. In our case, the pre-existing chronic basal ganglia infarcts may have contributed to the negative acute MRI findings. Given that our patient had chronic basal ganglia infarcts, the metabolic/vascular changes of hyperglycemia likely presented a second hit to the basal ganglia, explaining the uncommon presentation.Treatment of C-H-BG syndrome consists of managing the hyperglycemia with insulin, with the addition of dopamine antagonists for symptomatic relief. In our patient the chorea completely resolved with hyperglycemic control.
Conclusions: Though differential causes of chorea are wide, the quick resolution of chorea with the optimization of blood glucose highlights the importance of considering metabolic causes of new, sudden onset chorea in a diabetic. T1 hyperintensities in basal ganglia are characteristic imaging findings in C-H-BG, but the absence of acute imaging findings does not exclude the diagnosis. Chorea is an uncommon manifestation of a common medical condition and early identification can reduce morbidity and unnecessary medical testing.