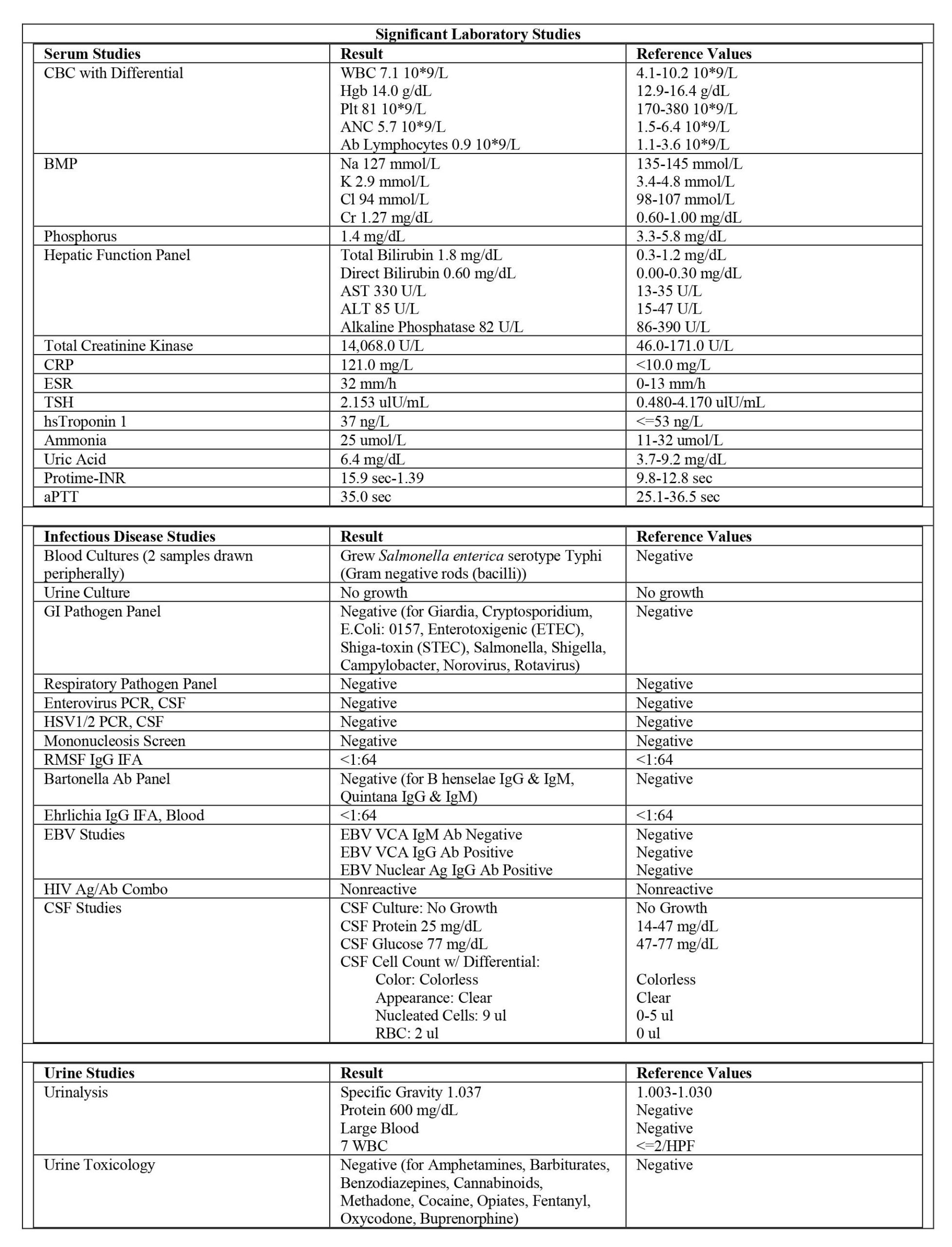
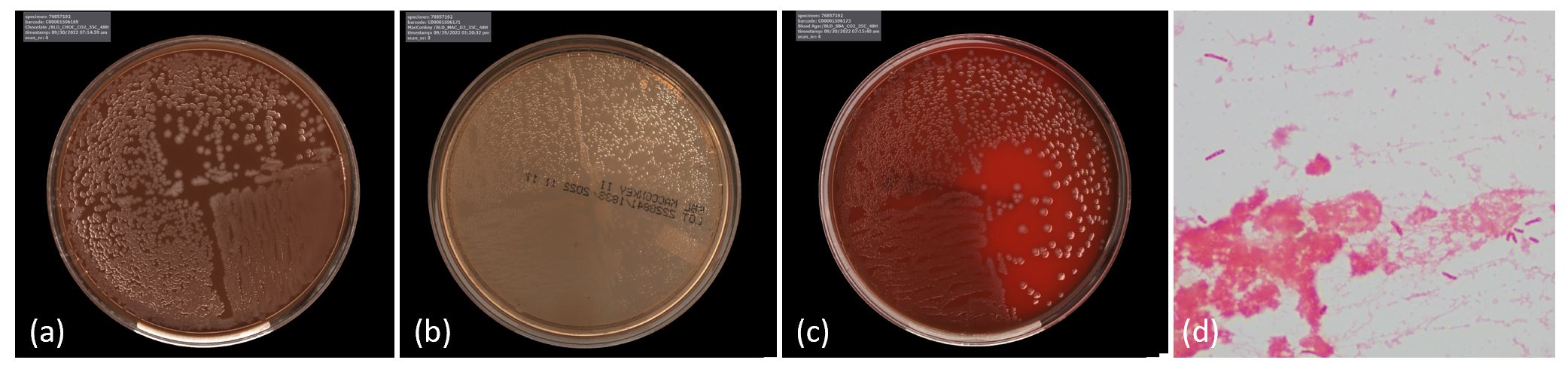
Case Presentation: A previously healthy, obese 15-year-old male presented to an ED in North Carolina with acute encephalopathy preceded by six days of flu-like symptoms with one day of diarrhea and cough. On presentation, he was febrile, tachycardic, tachypneic, with other vital signs normal. He was disoriented with slowed speech, inappropriate laughter, and delayed verbal responses. Parents had noted visual hallucinations and paranoia. There were no sick contacts and no personal or close contact travel history. Animal exposures were limited to a recent visit to a petting zoo, domesticated cats (with scratches on exam), and several insect bites. Initial evaluation was notable for elevated CK, myoglobinuria, acute kidney injury (AKI), hyponatremia, hypokalemia, transaminitis, thrombocytopenia, coagulopathy, and elevated inflammatory markers. Abdominal ultrasound revealed hepatosplenomegaly. Further lab workup, including CSF studies, were unremarkable (Table 1). Fluid resuscitation was initiated for rhabdomyolysis treatment with vancomycin, ceftriaxone, and doxycycline for broad bacterial and tick-borne illness coverage.During his hospitalization, his encephalopathy escalated to require sedation due to worsening hallucinations and aggressive behavior. He had non-bloody diarrhea; however, GI pathogen panel (GIPP) was negative. His blood cultures returned positive for gram negative rods (Figure 1) and ultimately speciated as pan-sensitive Salmonella enterica serotype typhi (S. typhi). He gradually returned to his baseline mental status with resolution of rhabdomyolysis and improvement in inflammatory markers and transaminitis. He was discharged having completed a full course of doxycycline for tick-borne illness and continued on ciprofloxacin to complete a treatment course for salmonella bacteremia.
Discussion: Neuropsychiatric manifestations of typhoid fever have been described but acute psychosis is rare and not well understood. In one study that detailed neuro-psychiatric complications in multidrug-resistant typhoid fever, impaired cognition and confusion were seen in 73.3% of cases, but acute psychosis was present in only 0.6% of cases [1]. Severe enteric fever can lead to “typhoid encephalopathy” characterized by altered mental status (AMS), confusion, and delirium, and has been described in up to 17% of cases in adults and children [2,3]. Rhabdomyolysis has been rarely described in enteric fever and is even more uncommon in typhoid fever [4]. As of 2021, only 19 cases of S. typhi-induced rhabdomyolysis have been described in the literature, with only four of those cases in pediatric patients [5]. Several mechanisms behind this pathophysiology have been proposed, including sepsis-induced hypoxic injury and direct bacterial invasion [4].The diagnosis of S. typhi in our case was unusual given the patient’s negative stool PCR and the absence of travel history. Of the 200-300 cases of S. typhi in the United States each year, approximately 80% of cases are travelers returning from endemic regions. As systemic symptoms arise, stool cultures are only positive in 30-40% of cases, compared to blood cultures which are positive in 40-80% of cases [2]. S. typhi is a significant public health concern and should be considered in a patient with diarrhea and AMS, even if recent travel is not endorsed and GIPP is negative [2].
Conclusions: This case describes a unique presentation of typhoid fever with acute psychosis and rhabdomyolysis in a patient without a history of travel and a negative GIPP.