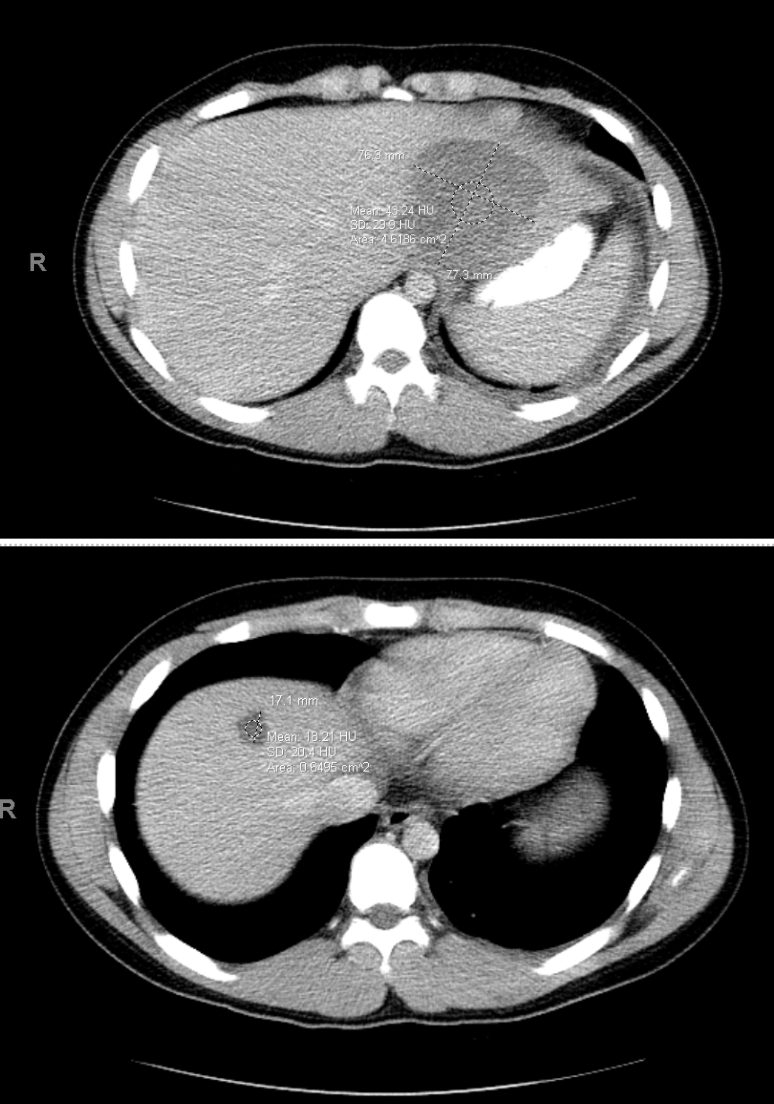
Case Presentation: A 14-year-old healthy male presented with throbbing, right sided abdominal pain, intermittent headache, and bilateral neck and shoulder pain in the setting of six days of fever (temperature max 103° F). He had a history of a normal endoscopy after elevated stool calprotectin that normalized without intervention. Exposure history was notable for freshwater swimming in the American River in Northern California, visiting a farm, petting a lizard, and a dental cavity filling two weeks prior to presentation. He had no prior surgery, biliary tract disease, or helminth infection. His physical exam was notable for discomfort at rest, diaphoresis, and diffusely tender abdomen with guarding and distension but without notable rigidity or rebound tenderness. His labs showed significant leukocytosis, mild transaminitis, urinalysis with proteinuria, CRP 33, ESR 91, negative blood culture; lipase, lactate, BMP, GGT, alkaline phosphatase and bilirubin were all within normal limits. Abdominal CT showed two liver lesions, left pleural effusion, and intussusception (Figures 1, 2). The patient was started on piperacillin/tazobactam. Interventional radiology drained 40 ml of foul-smelling and bloody drainage, followed by JP drain placement. The anaerobic culture was positive for Fusobacterium nucleatum. He completed six weeks of ertapenem followed by two weeks of metronidazole and showed improvement on imaging and a downtrend of inflammatory markers.
Discussion: Pyogenic liver abscesses can occur via direct extension of local infection or hematogenous spread through the hepatic artery or the portal vein from sources within the abdominal cavity. Fusobacterium liver abscesses are uncommon, and can be associated with Lemierre’s syndrome, gastroenteric pathology, or dental work. In Lemierre’s, the liver is the most common site of visceral involvement with liver abscesses occurring in 2-4% of cases (1). Lemierre’s was considered and ruled out with imaging. Intussusception and inflammatory bowel disease (IBD) were considered as possible causes for bacterial translocation into the abdominal cavity. It was felt that the intussusception was incidental in this case with no peritoneal signs on physical exam, and thus lower concern for mesenteric ischemia secondary to intussusception that could have contributed to a bacterial translocation. Liver abscess is a rare complication of IBD. In one review of adult literature, it was found that most liver abscesses as a complication of IBD occur in patients with longstanding and active Crohn’s disease (2). With negative prior work up and negative capsule endoscopy after discharge, IBD was ruled out in this case. As fusobacteria are normal oral flora, manipulation during dental procedures could have caused these curious liver abscesses via translocation of bacteria. To the best of our knowledge, there is only one other case report of an adolescent, immunocompetent patient with F. nucleatum as the cause of liver abscess (3), effectively making this the first pediatric case in current literature.
Conclusions: Immunocompetent children rarely present with liver abscesses secondary to dental procedures but require urgent diagnosis and treatment as this pathology can carry a high mortality. This case highlights the importance of keeping a broad differential as the cause of liver abscesses as well as the importance for ruling out potentially life threatening or chronic conditions that may be underlying this presentation.