Background: It is common practice to monitor QTc interval in hospitalized patients newly started on antipsychotics. While some guidelines exist for frequency of ordering EKGs in the outpatient setting, these may not apply to inpatients due to comorbid electrolyte disturbances or addition of other new medications. There are no evidence-based guidelines for QTc monitoring frequency in inpatients started on antipsychotics, which creates the potential for wasteful over-ordering or dangerous under-ordering of EKGs. This study seeks to examine EKG ordering and follow-up practices by hospitalists, residents and advanced practice providers to (1) ascertain whether these practitioners are providing uniform care and (2) assess the perceived utility of EKG results on medical management.
Methods: A survey was distributed by email to all hospitalists, internal medicine residents, and advanced practice providers working in the Department of Medicine at a large urban academic medical center. Items included the provider’s tendency to order baseline EKGs in patients newly started on antipsychotics, interval for obtaining follow-up EKGs, tendency to follow-up on results of ordered EKGs, and how frequently they felt that they used these results in clinical management.
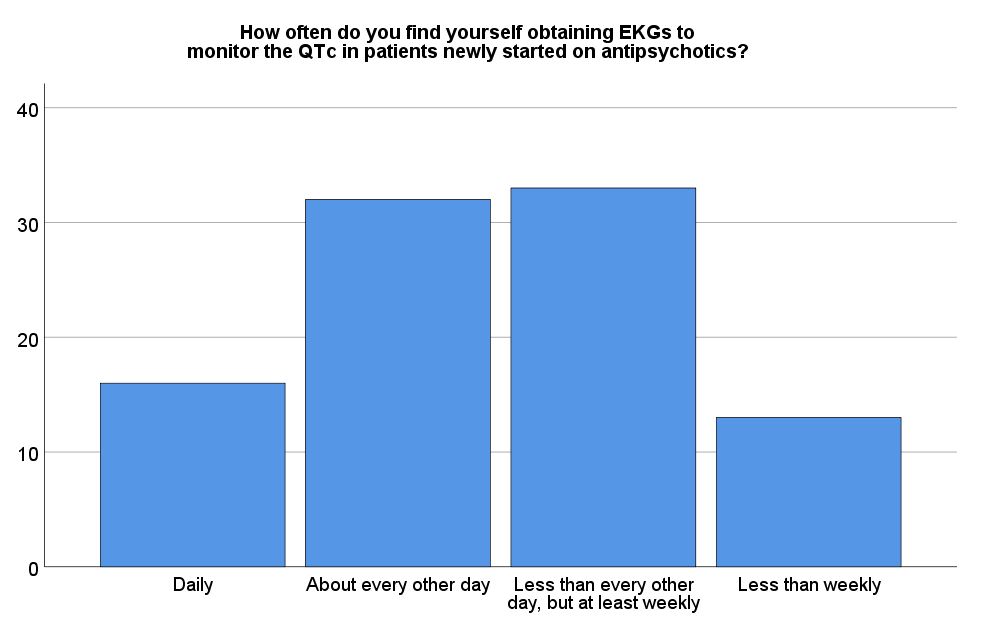
Results: Ninety-five individuals out of 226 (42.0%) responded to the survey, including 27 hospitalists, 58 residents, and 10 advanced practitioners. Seventy-one providers (74.7%) reported ordering baseline EKGs on every patient started on an antipsychotic. Frequency of monitoring varied widely; sixteen (16.8%) reported “daily” EKG ordering, 32 (33.7%) reported “about every other day,” 33 (34.7%) reported “less than every other day, but at least weekly,” and 13 (13.7%) reported “less than weekly” EKG ordering. Thirty-two respondents (33.7%) reported they did not routinely follow up on the results of EKGs they ordered. Additionally, twenty-nine of the physicians (34.1%) felt that EKG results were unlikely to be used in clinical management. Of note, hospitalists were significantly more likely to report that EKG results were not useful in clinical management compared to residents (OR = 6.52, p < .001).
Conclusions: There is widespread variation in EKG ordering habits among providers monitoring for QTc changes in patients newly started on antipsychotics. The lack of uniform ordering frequency of EKGs may lead to wasteful ordering of EKGs or under-monitoring for QTc prolongation. It is also concerning that 1/3 of providers do not regularly follow up on tests they have ordered, raising the potential for medicolegal risk. Finally, the majority of hospitalists felt that EKGs were not often useful in clinical management, in direct contrast to residents’ beliefs. These findings indicate there is a great need for further studies to inform new evidence-based guidelines recommending how often to order EKGs to monitor the QTc for inpatients newly started on antipsychotics.