Background: While NT-proBNP has been known to predict mortality in heart failure patients and in hospitalized patients, its association with mortality in healthy adults without a history of cardiovascular disease is unknown. Further, it is unclear if a one-time measurement of NT-proBNP can predict distant mortality. Therefore, we examined the association between NT-proBNP with all-cause and cause-specific mortality.
Methods: We used publicly available, continuous National Health and Nutrition Examination Survey (NHANES) data files from 1999-2004. We excluded individuals younger than 18 years, those with a history of coronary artery disease or congestive heart failure, and those with missing N-BNP values were excluded. We defined two categories of N-BNP: ≤125pg/mL and >125pg/mL based on recommendation of the Heart Failure societies of United States, Europe, and Japan. We used Cox proportional hazard models to determine hazard ratio without and with adjustment for age, gender, race, education attainment, household income to poverty threshold ratio, hypertension, diabetes, smoking, alcohol use, body mass index, serum cholesterol, and estimated glomerular filtration rate. To determine if the association between one-time measurement of NT-proBNP and subsequent risk of mortality changed during follow-up, we conducted two sensitivity analyses (1) piece-wise splines at 5, 10, 15 years and (2) restricted cubic splines with knots at 33% and 66% of follow up.
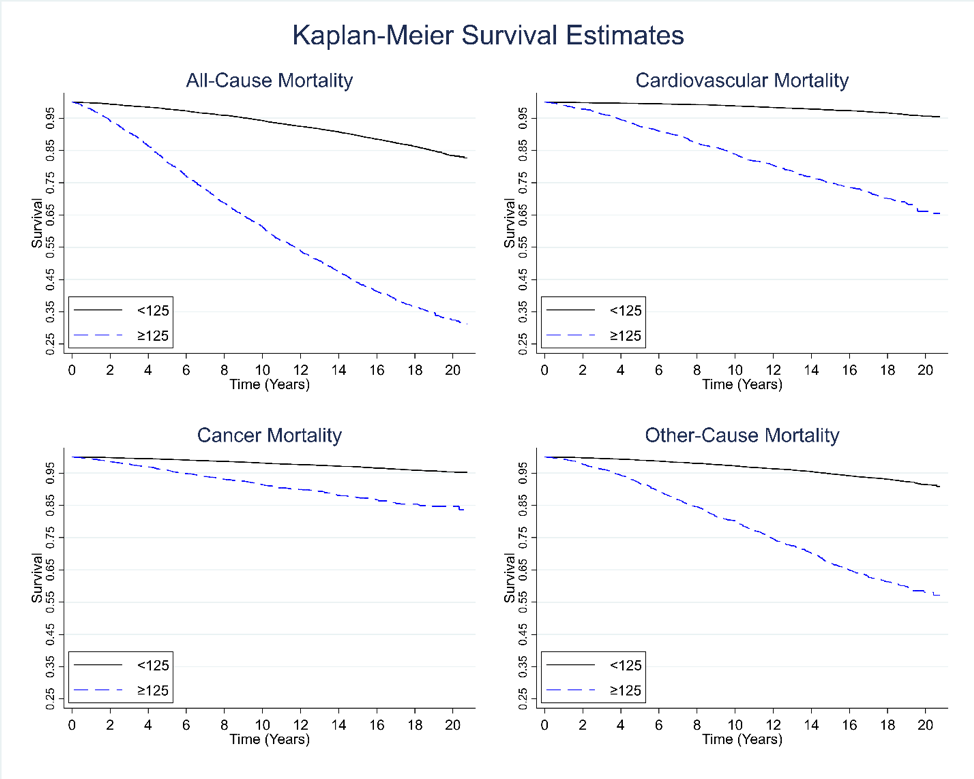
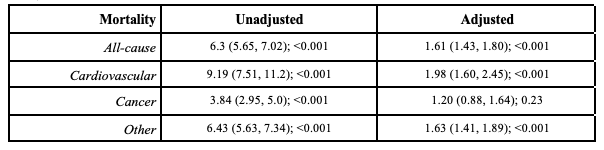
Results: Of the 12,933 participants, 6,832 (52.8%) were females, 2,480 (19.2%) were African Americans, and 2,801(21.7%) were older than 65 years. Median (IQR) of NT-proBNP was 43.7 (74.1) pg/mL and 2403(18.6%) participants had N-BNP >125pg/mL. During 206,353 person-years of follow-up, 2,959 (22.9%) participants died of which 875(6.8%) were due to cardiovascular diseases, 655(5.1%) were due to cancer, and 1,429 (11.0%) were due to other causes. Participants with NT-proBNP >125pg/mL had significantly higher all-cause, cardiovascular, cancer, and other-cause mortality (all P< 0.0001; Figure 1). In adjusted models, participants with NT-proBNP >125 had 61% higher risk of all-cause mortality, 98% higher risk of cardiovascular mortality, and 63% risk of other cause mortality but no association was noted with cancer mortality (Table). Furthermore, the adjusted hazard ratios did not change during follow-up in sensitivity analyses suggesting that the observed associations did not dilute during follow-up.
Conclusions: A single measurement of NT-proBNP is associated with increased mortality during a long-term follow-up in adult population free of coronary artery disease or heart failure. The underlying mechanisms for this association need further exploration.